低收入精神健康障碍患者补充和综合医学的使用
Mayo Clinic proceedings. Innovations, quality & outcomes
Pub Date : 2025-02-01
DOI:10.1016/j.mayocpiqo.2024.11.002
引用次数: 0
摘要
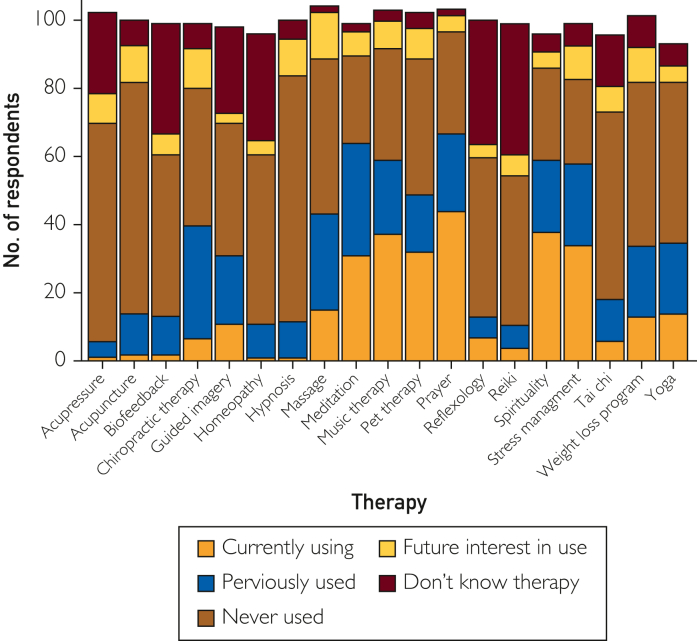
目的:评估有精神健康诊断的低收入人群中补充和综合医学(CIM)的使用情况,并评估基于CIM使用的健康社会决定因素(SDOH)的差异。患者和方法:我们在2020年8月11日至2021年11月18日期间,在明尼苏达州罗切斯特市的一家社区行为健康中心对门诊评估期间患有精神健康诊断和/或物质使用障碍的患者进行了调查。我们测量了当前CIM的知识、对未来使用CIM的兴趣以及SDOH。通过使用或不使用任何CIM来比较SDOH危险因素的平均数量的差异。结果:102例患者中,抑郁(87%)和焦虑(85%)的诊断较为常见。此外,72%的患者使用了至少1个CIM。最常见的三种方式是祈祷(41%),灵性(37%)和音乐(36%)。CIM的使用对情绪(49%)、压力(49%)和悲伤(43%)有明显的好处。三分之一的患者在常规治疗的基础上增加了CIM, 19%的患者报告说,传统医学治疗对他们的症状效果不佳。超过三分之二的人没有与医生讨论过他们使用CIM的情况。社会孤立和孤独很常见。使用CIM后,SDOH危险因素的数量确实有所不同。结论:祈祷、灵修和音乐是精神健康障碍患者经常使用的方法,被认为有助于缓解症状。CIM的使用与SDOH危险因素无关。整合CIM疗法可能有利于改善这一人群的心理健康。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Use of Complementary and Integrative Medicine Among Low-Income Persons With Mental Health Disorders
Objective
To evaluate the use of complementary and integrative medicine (CIM) among a low-income population with mental health diagnoses and to assess differences in social determinants of health (SDOH) on the basis of CIM use.
Patients and Methods
We surveyed patients with mental health diagnoses and/or substance use disorders during outpatient evaluations between August 11, 2020, and November 18, 2021, at a community behavioral health center in Rochester, MN. We measured knowledge of current CIM, interest in future use of CIM, and SDOH. Differences in mean number of SDOH risk factors were compared by use or nonuse of any CIM.
Results
Among 102 patients, depression (87%) and anxiety (85%) diagnoses were common. Moreover, 72% of patients used at least 1 CIM. The 3 most common modalities were prayer (41%), spirituality (37%), and music (36%). CIM use had perceived benefits for mood (49%), stress (49%), and sadness (43%). One-third of patients added CIM to conventional treatments, and 19% reported that traditional medical treatments did not work well for their symptoms. More than two-thirds had not discussed their use of CIM with their physicians. Social isolation and loneliness were common. The number of SDOH risk factors did differ by use of CIM.
Conclusion
Prayer, spirituality, and music are frequently used by patients with mental health disorders and were perceived to be helpful in relieving symptoms. CIM use was not related to SDOH risk factors. Integrating CIM therapies may be beneficial for improving mental health in this population.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Mayo Clinic proceedings. Innovations, quality & outcomes
Surgery, Critical Care and Intensive Care Medicine, Public Health and Health Policy
自引率
0.00%
发文量
0
审稿时长
49 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


