内部开发的基于深度学习的乳房体积调制弧线治疗自动规划工具的主动风险分析。
IF 3.3
Q2 ONCOLOGY
引用次数: 0
摘要
背景和目的:随着放射治疗领域内部创建的深度学习模型数量的增加,在临床使用之前,了解如何将与当地临床实施相关的风险降至最低是很重要的。本研究的目的是给出一个示例,说明如何在包含基于深度学习的乳房体积调制弧线疗法规划工具的实施工作流中识别风险并找到缓解策略,以降低这些风险。材料和方法:深度学习模型在私有谷歌云环境上运行,以获得足够的计算能力,并集成到可以在临床治疗计划系统(TPS)中启动的工作流中。一个多学科团队进行了主动失效模式和影响分析(FMEA),包括医生、物理学家、剂量师、技术人员、质量管理人员和研发团队。进一步检查了风险矩阵中被分类为“不可接受”和“可容忍”的失效模式,以找到缓解策略。结果:总共为整个工作流程定义了39种失效模式,分为四个步骤。其中33项为“可接受”,5项为“可接受”,1项为“不可接受”。缓解策略,例如特定案例的质量保证报告、附加脚本化检查和属性、弹出窗口和时间戳分析,将故障模式减少到两个“可容忍”区域,而在“不可接受”区域中没有故障模式。结论:前瞻性风险分析揭示了实施的工作流程中可能存在的风险,并导致实施降低风险评分的缓解策略,以提高临床使用的安全性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Pro-active risk analysis of an in-house developed deep learning based autoplanning tool for breast Volumetric Modulated Arc Therapy
Background and Purpose:
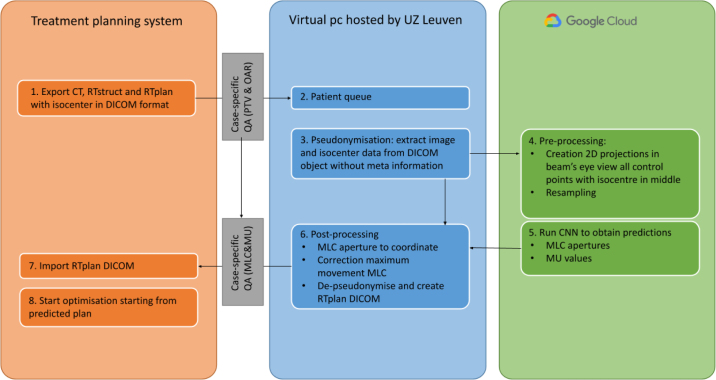
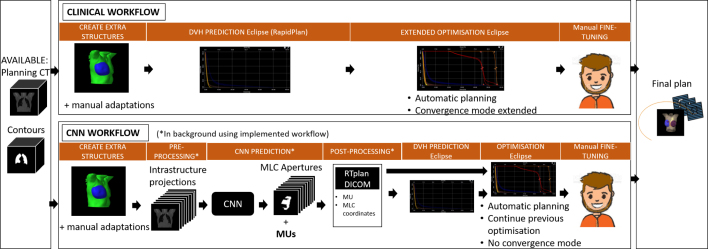
With the increasing amount of in-house created deep learning models in radiotherapy, it is important to know how to minimise the risks associated with the local clinical implementation prior to clinical use. The goal of this study is to give an example of how to identify the risks and find mitigation strategies to reduce these risks in an implemented workflow containing a deep learning based planning tool for breast Volumetric Modulated Arc Therapy.
Materials and Methods:
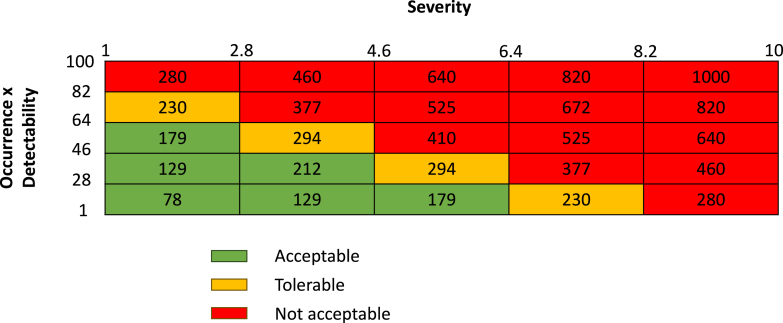
The deep learning model ran on a private Google Cloud environment for adequate computational capacity and was integrated into a workflow that could be initiated within the clinical Treatment Planning System (TPS). A proactive Failure Mode and Effect Analysis (FMEA) was conducted by a multidisciplinary team, including physicians, physicists, dosimetrists, technologists, quality managers, and the research and development team. Failure modes categorised as ‘Not acceptable’ and ‘Tolerable’ on the risk matrix were further examined to find mitigation strategies.
Results:
In total, 39 failure modes were defined for the total workflow, divided over four steps. Of these, 33 were deemed ‘Acceptable’, five ‘Tolerable’, and one ‘Not acceptable’. Mitigation strategies, such as a case-specific Quality Assurance report, additional scripted checks and properties, a pop-up window, and time stamp analysis, reduced the failure modes to two ‘Tolerable’ and none in the ‘Not acceptable’ region.
Conclusions:
The pro-active risk analysis revealed possible risks in the implemented workflow and led to the implementation of mitigation strategies that decreased the risk scores for safer clinical use.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Physics and Imaging in Radiation Oncology
Physics and Astronomy-Radiation
CiteScore
5.30
自引率
18.90%
发文量
93
审稿时长
6 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


