简要报告:不平等:KRAS突变亚型在非小细胞肺癌免疫治疗中的生存差异。
IF 3.5
Q2 ONCOLOGY
引用次数: 0
摘要
不同KRAS突变(KRASm)亚型在转移性NSCLC中的预测和预后意义尚未明确定义。我们使用了一个全国性的观察性数据库来研究KRASm亚型与基于免疫检查点抑制剂(ICI)治疗的转移性非小细胞肺癌的生存率之间的关系是否存在差异,跨越程序性死亡配体1 (PD-L1)水平。方法:纳入2016年至2021年接受一线ci治疗的晚期非鳞状NSCLC患者,这些患者已知PD-L1表达和KRAS、STK11、KEAP1和TP53等综合基因组图谱。在PD-L1表达亚组内(KRASm亚型(G12C, G12V, G12D,其他KRASm)和总生存率,使用Kaplan-Meier方法估计。结果:1539例患者中KRAS野生型(KRASwt) 819例,KRASm为720例(KRAS G12C 296例,KRAS G12V 143例,KRAS G12D 97例,其他KRASm 184例)。在50%或更高PD-L1亚组中,KRAS G12V患者的生存期(中位总生存期[mOS] = 8.2个月)比KRASwt (mOS = 13.3个月)和其他KRAS亚组(mOS范围为13.4至19.9个月)更差。经校正Cox多变量回归分析,在PD-L1≥50%亚组中,与KRASwt和其他KRASm亚型相比,KRAS G12V的死亡风险比为1.53 ~ 1.78(均p < 0.05)。结论:虽然50%或更高PD-L1的KRAS G12C、G12D和其他亚型患者的生存率与KRASwt相似,但KRAS G12V的生存率明显低于KRASwt和其他KRASm亚型。即使PD-L1高表达,也不应将所有KRASm视为ICI反应性的统一预测因子;KRAS G12V肿瘤在基于ci的治疗中可能有更差的结果,并从治疗强化中获益。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Brief Report: Not Created Equal: Survival Differences by KRAS Mutation Subtype in NSCLC Treated With Immunotherapy
Introduction
The predictive and prognostic implications of different KRAS mutation (KRASm) subtypes in metastatic NSCLC have not been clearly defined. We used a nationwide observational database to investigate whether KRASm subtypes differ in their association with survival in metastatic NSCLC treated with immune checkpoint inhibitor (ICI)-based therapy, across programmed death-ligand 1 (PD-L1) levels.
Methods
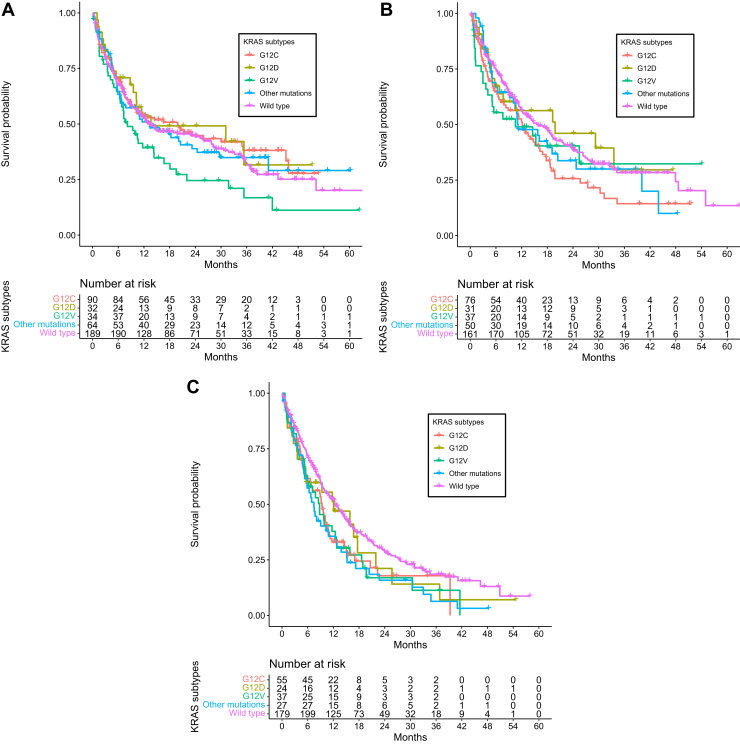
Patients with advanced nonsquamous NSCLC who initiated first-line ICI-based therapy from 2016 to 2021 and had known PD-L1 expression and comprehensive genomic profiling including KRAS, STK11, KEAP1, and TP53 were included. Within PD-L1 expression subgroups (<1%, 1%–49%, ≥50%), Cox multivariable regression was used to evaluate the association between KRASm subtypes (G12C, G12V, G12D, other KRASm) and overall survival, estimated using Kaplan-Meier methodology.
Results
Among the 1539 patients, 819 patients were KRAS wild type (KRASwt) and 720 were KRASm (296 KRAS G12C, 143 KRAS G12V, 97 KRAS G12D, 184 other KRASm). In the 50% or higher PD-L1 subgroup, patients with KRAS G12V had worse survival (median overall survival [mOS] = 8.2 mo) compared with KRASwt (mOS = 13.3 mo) and other KRAS subgroups (mOS ranging from 13.4 to 19.9 mo). On adjusted Cox multivariable regression in the 50% or higher PD-L1 subgroup, the hazard ratio for death for KRAS G12V ranged from 1.53 to 1.78 compared with KRASwt and other KRASm subtypes (all p < 0.05).
Conclusions
Although patients with 50% or higher PD-L1 with KRAS G12C, G12D, and other subtypes exhibited similar survival to KRASwt, KRAS G12V was associated with significantly worse survival than KRASwt and other KRASm subtypes. All KRASm should not be regarded as uniform predictors of ICI responsiveness, even with high PD-L1 expression; KRAS G12V tumors may have worse outcomes with ICI-based therapy and benefit from treatment intensification.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

JTO Clinical and Research Reports
Medicine-Oncology
CiteScore
4.20
自引率
0.00%
发文量
145
审稿时长
19 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


