埃塞俄比亚Debre Tabor综合专科医院成人急诊科分诊分类实施审计。
IF 1.2
4区 医学
Q3 EMERGENCY MEDICINE
引用次数: 0
摘要
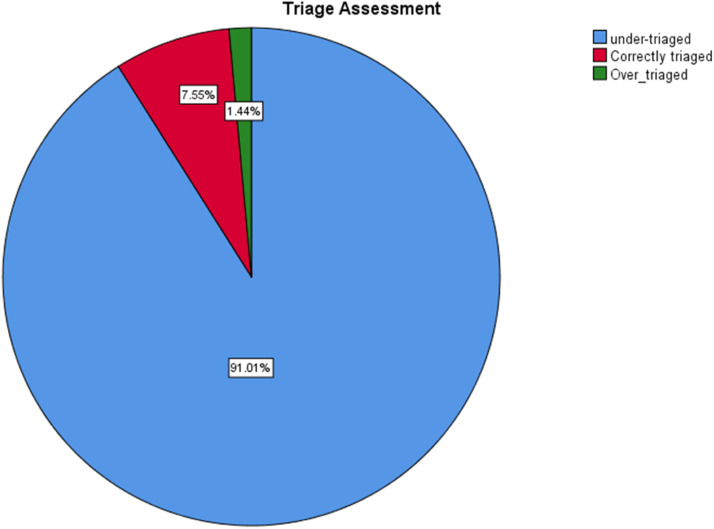
简介:在急诊室,分诊是决定患者临床急迫性的关键因素。分诊可以决定资源的使用和病人需要的治疗。许多患者就诊时间过晚,浪费了资源和时间,有些患者甚至可能在没有被看到的情况下出院,冒着生命危险。本研究旨在确定分诊工具是否完全完成、适当测量和记录,分诊早期预警评分(TEWS)是否计算,以及患者是否在适当的区域进行检查、分配和管理。方法:采用简单随机抽样的方法,选取2021年1月1日至2023年12月31日在Debre Tabor综合专科医院成人急诊科就诊的患者的病历,进行基于机构的横断面研究和回顾性图表回顾。采用描述性统计来描述个体变量,并使用交叉表来查看个体患者相关因素与其最终分诊状态之间的关系。结果:在随机选取的345例患者的病历中,67例(19.4%)未包含分诊单。只有21例(7.6%)患者的分诊预警总分计算正确,分诊正确。多数患者分诊不当(92.4%,n = 257),其中分诊不足253例(91%),分诊过度4例(1.4%)。Fischer的精确检验显示,患者的颜色编码类别、分诊早期预警评分文件与临床鉴别器的使用和最终分诊评估之间存在统计学上显著的关系(p = 0.007, p = 0.000, p = 0.000)。结论:我国分诊实施的现状令人担忧,特别是分诊不足的程度。关于临床鉴别器和TEWS计算的应用存在显著的差距。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Triage implementation audit at the adult emergency department of Debre Tabor Comprehensive Specialized Hospital in Ethiopia
Introduction
In an emergency room, triage is a crucial element that determines the clinical urgency of patients. Triage can dictate important decisions on the use of resources and the treatment that patients need. Many patients are seen later than necessary, wasting resources and time, and some may even be discharged without being seen, risking their lives. This study aimed to determine whether the triage tool was fully completed, properly measured, and documented, the triage early warning score (TEWS) was calculated, and whether patients were examined, distributed, and managed in appropriate areas.
Methods
An institution-based cross-sectional study with a retrospective chart review was conducted at Debre Tabor Comprehensive Specialized Hospital by selecting patients’ charts using simple random sampling among patients who visited the adult Emergency Department from January 1, 2021, to December 31, 2023. The descriptive statistics were presented to characterize individual variables, and cross-tabulation was used to see the relationship between individual patient-related factors and their final triage status.
Results
From the randomly selected 345 patients’ charts, 67 (19.4 %) didn't contain a triage sheet. The total triage early warning score was correctly calculated for only 21 (7.6 %) patients and properly triaged. Most of the patients were improperly triaged (92.4 %, n = 257), of which 253 (91 %) were under-triaged and four (1.4 %) were over-triaged. Fischer's exact test revealed a statistically significant relationship between patients’ color-coding category, triage early warning score documentation, and the use of clinical discriminators and final triage assessment (p = 0.007, p = 0.000, and p = 0.000 respectively).
Conclusion
The status of our triage implementation is alarming and specifically the level of under-triage. There is a significant gap regarding the application of clinical discriminators and TEWS calculations.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

African Journal of Emergency Medicine
EMERGENCY MEDICINE-
CiteScore
2.40
自引率
7.70%
发文量
78
审稿时长
85 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


