精神分裂症或心境障碍患者迟发性运动障碍的药物干预的疗效和可接受性:一项系统综述和网络荟萃分析
IF 9.6
1区 医学
Q1 BIOCHEMISTRY & MOLECULAR BIOLOGY
引用次数: 0
摘要
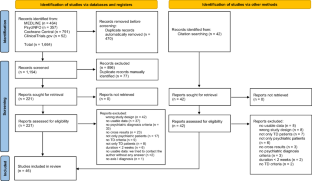
接触多巴胺受体拮抗剂(DRAs)的人可能会出现迟发性运动障碍(TD)。其临床治疗仍具有挑战性。我们通过搜索 PubMed/MEDLINE/PsycINFO/ClinicalTrials.gov/Cochrane Central Register(2023 年 5 月 22 日,预定义方案 https://osf.io/b52ae/)进行了一项系统性综述/随机效应网络荟萃分析(NMA),以了解针对精神分裂症或情绪障碍成人患者中 DRA 引起的 TD 的药物/脑刺激干预的随机对照试验(RCT)。主要结果为TD症状变化(标准化平均差/SMD)和全因停药(可接受性风险比/RR)。进行了敏感性分析。对整体、局部不一致性、偏倚风险(RoB-2 工具)和证据置信度(CINeMA)进行了测量。我们纳入了 46 项试验(n = 2844,年龄 = 52.89 ± 9.94 岁,男性 = 59.8%,精神分裂症 = 84.6%,心境障碍 = 15.4%),所有试验均为药物干预与安慰剂对比试验。我们发现了三个子网络。在网络1中,几种治疗方法对TD症状的疗效优于安慰剂,且具有较大的效应量(k = 34,n = 2269),包括22项干预措施与安慰剂的比较,但18项仅有1项RCT,15项的n≤20。出现了高度异质性(I2 = 57.1%;tau2 = 0.0797)和总体不一致性(Q = 32.64;df = 14;p = 0.0032)。在可接受性方面没有出现明显差异。如果将分析范围限制在具有 n > 20 项试验和 > 1 项 RCT 的治疗方法,则只有戊苯那嗪(k = 5,SMD = -0.69;95% CI = -1.00, -0.37)和维生素 E(k = 7,SMD = -0.49;95% CI = -0.87, -0.11)优于安慰剂。考虑到AIMS评分,仅在偏倚风险较低的试验中,24/36毫克(k = 2,SMD = -0.57/-0.60)的去甲替拉嗪的疗效优于安慰剂。去甲替拉嗪和戊苯那嗪的研究结果可信度较低,所有其他药物的可信度都很低。在网络 2(k = 2,n = 63)中,改用莫林酮(k = 1,n = 9)与改用氟哌啶醇相比,TD 会恶化(SMD = 1.68;95% CI = 0.61,2.76)。在网络3(k = 3,n = 194)中,抗精神病药物洗脱+安慰剂(k = 1,n = 25)与TAU+安慰剂(k = 1,n = 27)相比,TD恶化(SMD = 1.30;95% CI = 0.36,2.23)。尽管一些质量/置信度很低的治疗方法的效应大小很大,但如果考虑到质量较高的证据,只有戊苯那嗪或去甲替拉嗪是循证的TD一线治疗方法,维生素E可能是二线治疗方法。应避免转用吗丁啉酮和抗精神病药物冲洗。我们需要更多的治疗方案和更高质量的试验。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Efficacy and acceptability of pharmacological interventions for tardive dyskinesia in people with schizophrenia or mood disorders: a systematic review and network meta-analysis
Tardive Dyskinesia (TD) can occur in people exposed to dopamine receptor antagonists (DRAs). Its clinical management remains challenging. We conducted a systematic review/random-effects network meta-analysis (NMA) searching PubMed/MEDLINE/PsycINFO/ClinicalTrials.gov/Cochrane Central Register (22/05/2023, pre-defined protocol https://osf.io/b52ae/ ), for randomized controlled trials (RCTs) of pharmacological/brain stimulation interventions for DRA-induced TD in adults with schizophrenia or mood disorders. Primary outcomes were TD symptom change (standardized mean difference/SMD) and all-cause discontinuation (acceptability-risk ratio/RR). Sensitivity analyses were conducted. Global, local inconsistencies, risk of bias (RoB-2 tool), and confidence in evidence (CINeMA) were measured. We included 46 trials (n = 2844, age = 52.89 ± 9.94 years, males = 59.8%, schizophrenia = 84.6%, mood disorders = 15.4%), all testing pharmacological interventions versus placebo. We identified three subnetworks. In network 1, several treatments outperformed placebo on TD symptoms with large effect sizes (k = 34, n = 2269), encompassing 22 interventions versus placebo, but 18 had 1 RCTs only, and 15 had n ≤ 20. High heterogeneity (I2 = 57.1%; tau2 = 0.0797), and global inconsistency (Q = 32.64; df = 14; p = 0.0032) emerged. No significant differences emerged in acceptability. When restricting analyses to treatments with trials with n > 20 and >1 RCT, only valbenazine (k = 5, SMD = −0.69; 95% CI = −1.00, −0.37) and vitamin E (k = 7, SMD = −0.49; 95% CI = −0.87, −0.11) were superior to placebo. Deutetrabenazine outperformed placebo considering AIMS score and in low risk of bias trials only and with a moderate effect size for 24/36 mg (k = 2, SMD = −0.57/−0.60). Confidence in findings was low for deutetrabenazine and valbenazine, very low for all others. In network 2 (k = 2, n = 63), switch to molindone (k = 1, n = 9) versus switch to haloperidol worsened TD (SMD = 1.68; 95% CI = 0.61,2.76). In network 3 (k = 3, n = 194), antipsychotic wash-out+placebo (k = 1, n = 25) versus TAU+placebo (k = 1, n = 27) worsened TD (SMD = 1.30; 95% CI = 0.36,2.23). Despite large effect sizes for some treatments with very low quality/confidence, when considering higher quality evidence only valbenazine or deutetrabenazine are evidence-based first-line treatments for TD, and potentially vitamin E as second-line. Switching to molindone and antipsychotic washout should be avoided. More treatment options and higher-quality trials are needed.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Molecular Psychiatry
医学-精神病学
CiteScore
20.50
自引率
4.50%
发文量
459
审稿时长
4-8 weeks
期刊介绍:
Molecular Psychiatry focuses on publishing research that aims to uncover the biological mechanisms behind psychiatric disorders and their treatment. The journal emphasizes studies that bridge pre-clinical and clinical research, covering cellular, molecular, integrative, clinical, imaging, and psychopharmacology levels.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


