以患者和家庭为中心的护理干预对重症监护病房结果的影响:随机对照试验的荟萃分析。
IF 1.9
4区 医学
Q2 ANESTHESIOLOGY
引用次数: 0
摘要
背景:以患者和家庭为中心的护理(PFCC)干预措施越来越被认为是解决重症监护病房(icu)患者各种心理健康问题的可行方法。因此,本综述旨在评估以患者和家庭为中心的护理干预对入住重症监护病房(icu)的成年患者特定结局的影响。方法:我们系统地检索了四个主要数据库的平行组随机对照试验(RCTs)。使用PRISMA框架报告我们的审查。我们纳入了icu收治的成年患者(18岁)的研究,并检查了任何类型的以患者和家庭为中心的护理干预(PFCC)对抑郁、焦虑、谵妄和住院时间等结果的影响。数据提取由Medline,谷歌Scholar和ScienceDirect的两位作者独立完成,从成立到2024年7月。采用随机效应模型对数据进行汇总。结果:我们的系统评价和荟萃分析共纳入了11项研究,总样本量为3352例患者(PFCC组,n = 1681;常规护理组,n = 1671)。随机效应模型显示PFCC组谵妄患病率显著降低,合并风险比(RR)为0.54 (95% CI 0.36 ~ 0.81)。然而,其他结果如抑郁、ICU住院时间和焦虑没有统计学意义。值得注意的是,所有纳入的研究都被评估为具有高偏倚风险或不明确的偏倚风险。结论:PFCC干预可显著降低ICU患者谵妄发生率;然而,它们对其他结果的影响,如抑郁、焦虑和住院时间,在统计上并不显著。本文章由计算机程序翻译,如有差异,请以英文原文为准。
The impact of patient- and family-centered care interventions on intensive care unit outcomes: a meta-analysis of randomized controlled trials
Background
Patient and Family-Centered Care (PFCC) interventions are increasingly recognized as a viable approach to address various mental health issues among patients in Intensive Care Units (ICUs). Therefore, this review aims to estimate the effect of Patient and Family-Centered Care Interventions on specific outcomes in adult patients admitted to Intensive Care Units (ICUs).
Methods
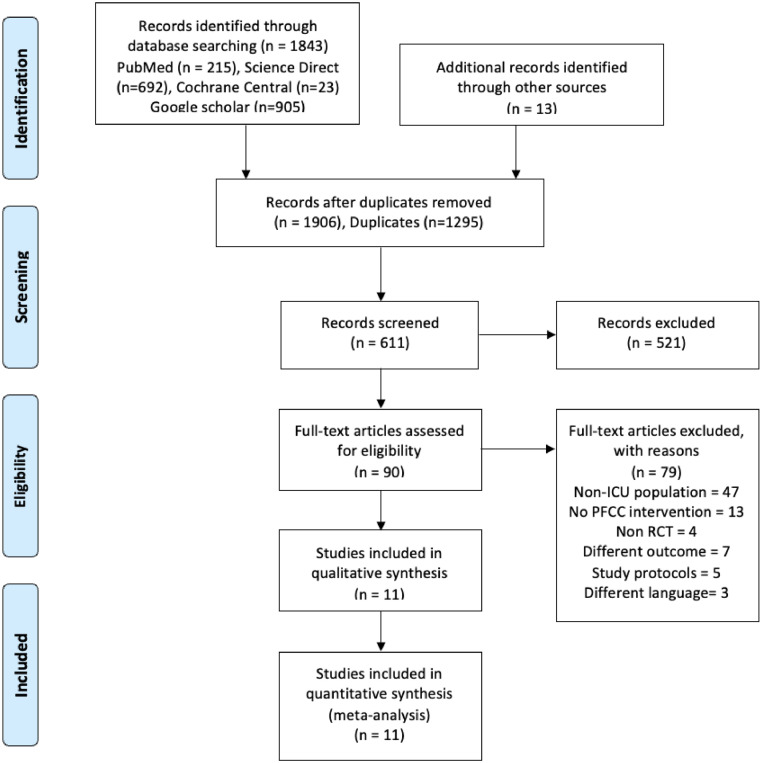
We systematically searched four major databases for parallel arm Randomized Controlled Trials (RCTs). The PRISMA framework was used to report our review. We included studies involving adult patients (> 18-years) admitted to ICUs and examined the effects of any type of Patient and Family-Centered Care intervention (PFCC) on outcomes such as depression, anxiety, delirium, and length of hospital stay. Data extraction was performed independently by two authors in Medline, Google Scholar, and ScienceDirect, from inception to July 2024. Random effects model was used to pool the data.
Results
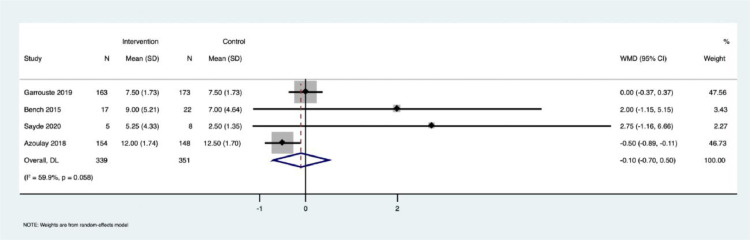
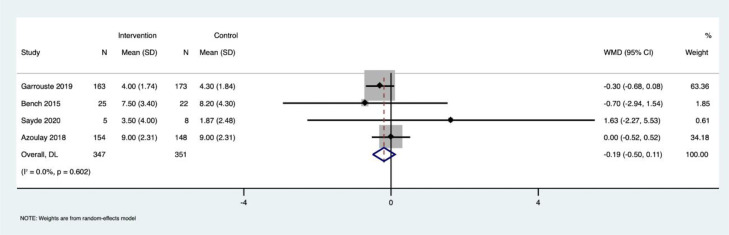
A total of 11 studies were included in our systematic review and meta-analysis, with a combined sample size of 3352 patients (PFCC group, n = 1681; usual care group, n = 1671). A random-effects model revealed a significant reduction in delirium prevalence in the PFCC group, with a pooled Risk Ratio (RR) of 0.54 (95% CI 0.36 to 0.81). However, no statistical significance was found for other outcomes such as depression, length of ICU stay, and anxiety. It is important to note that all the included studies were assessed to have either a high or unclear risk of bias.
Conclusion
PFCC interventions may significantly reduce delirium rates among ICU patients; however, their effects on other outcomes, such as depression, anxiety, and length of stay, were not statistically significant.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Brazilian Journal of Anesthesiology
ANESTHESIOLOGY-
CiteScore
2.10
自引率
0.00%
发文量
88
审稿时长
68 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


