儿童、成人和晚期多发性硬化症患者:对临床特征和治疗反应的统一分析
IF 2.9
3区 医学
Q2 CLINICAL NEUROLOGY
引用次数: 0
摘要
目的 本研究旨在对儿童发病型多发性硬化症(POMS)、成人发病型多发性硬化症(AOMS)和晚期发病型多发性硬化症(LOMS)患者的临床特征、疾病进展和治疗反应进行统一分析比较。方法 我们采用回顾性队列设计,分析了多发性硬化症诊所 269 名患者的病历,并根据诊断时的年龄将其分为 POMS 组(18 岁)、AOMS 组(≥18 岁和 50 岁)和 LOMS 组(≥50 岁)。数据收集的重点是人口统计学、临床表现、残疾评分、核磁共振成像结果和治疗结果。结果我们的研究结果表明,虽然所有组别中女性始终占多数,但吸烟习惯不同,疾病的发病和发展也存在差异。发病情况存在很大差异,38.5%的LOMS患者为进行性发病。从POMS组到LOMS组,残疾评分均有所上升,基线平均EDSS评分为1.81分,而LOMS组目前的EDSS评分最高,为3.33分。LOMS组的ARR更高。脑干和脊髓病变在POMS和LOMS患者中更为常见,但差异无统计学意义。在接受检测的患者中,89.6%呈OCB阳性。患者明显转向二线疗法,尤其是在LOMS患者中,有49.1%的患者在接受初始DMT治疗后病情得到控制。59.7%的POMS患者、47%的AOMS患者和38.5%的LOMS患者的病情得到了控制。结论POMS、AOMS和LOMS患者的临床特征和治疗反应存在显著差异,这突出表明了针对不同年龄段的多发性硬化症管理策略的必要性,同时也强调了LOMS患者所面临的独特挑战。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Pediatric, adult, and late-onset multiple sclerosis patients: A unified analysis of clinical profiles and treatment responses
Objective
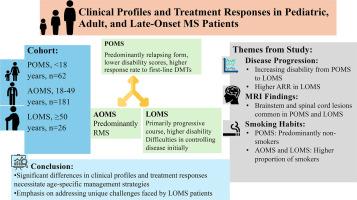
This study aimed to conduct a unified analysis comparing the clinical characteristics, disease progression, and treatment responses of pediatric-onset multiple sclerosis (POMS), adult-onset multiple sclerosis (AOMS), and late-onset multiple sclerosis (LOMS) patients.
Methods
Utilizing a retrospective cohort design, we analyzed the records of 269 patients from MS clinics and categorized them into the POMS (<18 years), AOMS (≥18 and <50 years), and LOMS (≥50 years) groups based on age at diagnosis. Data collection focused on demographics, clinical manifestations, disability scores, MRI findings, and treatment outcomes.
Results
Our findings indicate that while there was a consistent female majority across all groups, distinct smoking habits and differences in disease onset and progression were observed. Disease onset showed substantial differences, with 38.5 % of LOMS patients having a progressive onset. Disability scores increased from the POMS to the LOMS, with a baseline mean EDSS score of 1.81, and the LOMS group had the highest current EDSS score of 3.33. The ARR was greater in the LOMS group. Brainstem and spinal cord lesions were more common in patients with POMS and LOMS, but the difference was not statistically significant. Among those tested, 89.6 % showed OCB positivity. There was a notable shift toward second-line therapies, especially among LOMS patients, with 49.1 % achieving disease control with their initial DMT. Disease control was achieved by 59.7 % of the POMS patients, 47 % of the AOMS patients, and 38.5 % of the LOMS patients. Progression independent of relapse activity (PIRA) was observed in 19.7 % of patients, with higher second-line treatment requirements and higher EDSS scores in the PIRA group.
Conclusion
Significant differences in clinical profiles and treatment responses among POMS, AOMS, and LOMS patients underscore the necessity for age-specific management strategies for MS, emphasizing the unique challenges faced by LOMS patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Multiple sclerosis and related disorders
CLINICAL NEUROLOGY-
CiteScore
5.80
自引率
20.00%
发文量
814
审稿时长
66 days
期刊介绍:
Multiple Sclerosis is an area of ever expanding research and escalating publications. Multiple Sclerosis and Related Disorders is a wide ranging international journal supported by key researchers from all neuroscience domains that focus on MS and associated disease of the central nervous system. The primary aim of this new journal is the rapid publication of high quality original research in the field. Important secondary aims will be timely updates and editorials on important scientific and clinical care advances, controversies in the field, and invited opinion articles from current thought leaders on topical issues. One section of the journal will focus on teaching, written to enhance the practice of community and academic neurologists involved in the care of MS patients. Summaries of key articles written for a lay audience will be provided as an on-line resource.
A team of four chief editors is supported by leading section editors who will commission and appraise original and review articles concerning: clinical neurology, neuroimaging, neuropathology, neuroepidemiology, therapeutics, genetics / transcriptomics, experimental models, neuroimmunology, biomarkers, neuropsychology, neurorehabilitation, measurement scales, teaching, neuroethics and lay communication.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


