重症介入治疗后患者的用药模式和潜在的药物相互作用:伊朗的一项研究。
IF 3.5
3区 医学
Q2 PHARMACOLOGY & PHARMACY
引用次数: 0
摘要
背景:经皮冠状动脉介入治疗(PCI)后的患者通常需要复杂的药物治疗方案来预防不良心血管事件的发生。然而,这些治疗方案可能会导致潜在的药物相互作用(pDDIs)和多重用药,给临床带来巨大挑战。本研究旨在评估伊朗设拉子市做完冠状动脉造影术的患者的用药模式、pDDIs 和多重用药的发生率及相关性:对设拉子的 9019 名 PCI 患者进行了横断面研究。收集并分析了包括人口统计学、病史和药物清单在内的患者数据。应用解剖治疗化学(ATC)分类系统,使用 Lexicomp 数据库识别 pDDIs,并对其严重程度进行分类。使用多变量模型评估了与重大 pDDIs 和多重用药相关的因素:研究发现,91.6%的患者接受了他汀类药物处方,94.5%的患者接受了抗血小板治疗。值得注意的是,82.8%的患者被确认至少有一种 pDDI,其中 80.4%有明显的相互作用(C、D 或 X 类)。常见的潜在相互作用包括阿司匹林与氯吡格雷和洛伐他汀。73.6%的患者普遍使用多种药物,这与较高的相互作用风险有关。多药合用、男性、糖尿病和心力衰竭等因素是预测 pDDIs 的重要因素:该研究强调了PCI术后患者中pDDIs和多种药物的高发病率,揭示了临床指南与药物相互作用数据库之间存在的重要差距。更新相互作用数据库以反映当前的临床实践,加强数据库开发者与指南作者之间的合作,对于改善用药安全和患者预后至关重要。本文章由计算机程序翻译,如有差异,请以英文原文为准。
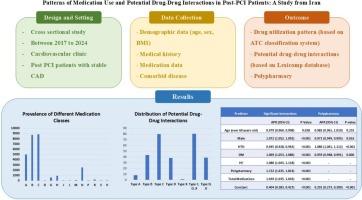
Patterns of medication use and potential drug-drug interactions in post-PCI patients: A study from Iran
Background
Post-percutaneous coronary intervention (PCI) patients often require complex medication regimens to prevent adverse cardiovascular events. However, these regimens can lead to potential drug-drug interactions (pDDIs) and polypharmacy, posing significant clinical challenges. This study aims to evaluate the pattern of medication use, prevalence, and correlates of pDDIs and polypharmacy among post-PCI patients in Shiraz, Iran.
Methods
A cross-sectional study was conducted on 9019 PCI patients in Shiraz. Patient data, including demographics, medical history, and medication lists, were collected and analyzed. The Anatomical Therapeutic Chemical (ATC) classification system was applied. pDDIs were identified using the Lexicomp database, and their severity was classified. Factors associated with significant pDDIs and polypharmacy were assessed using multivariable modeling.
Results
The study found that 91.6 % of patients received statin prescriptions and 94.5 % were on antiplatelet therapy. Notably, 82.8 % were identified with at least one pDDI, with 80.4 % having significant interactions (Categories C, D, or X). Common potential interactions included aspirin with clopidogrel and rosuvastatin. Polypharmacy was prevalent in 73.6 % of patients, associated with higher risks of interactions. Factors such as polypharmacy, male gender, diabetes mellitus, and heart failure were significant predictors of pDDIs.
Conclusions
The study underscores the high prevalence of pDDIs and polypharmacy among post-PCI patients, revealing a critical gap between clinical guidelines and drug interaction databases. Updating interaction databases to reflect current clinical practices and enhancing collaboration between database developers and guideline authors are essential for improving medication safety and patient outcomes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Vascular pharmacology
医学-药学
CiteScore
6.60
自引率
2.50%
发文量
153
审稿时长
31 days
期刊介绍:
Vascular Pharmacology publishes papers, which contains results of all aspects of biology and pharmacology of the vascular system.
Papers are encouraged in basic, translational and clinical aspects of Vascular Biology and Pharmacology, utilizing approaches ranging from molecular biology to integrative physiology. All papers are in English.
The Journal publishes review articles which include vascular aspects of thrombosis, inflammation, cell signalling, atherosclerosis, and lipid metabolism.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


