儿童狼疮相关低凝血酶原血症综合征:感染后症状与自身免疫症状的区别
IF 3.7
3区 医学
Q1 HEMATOLOGY
引用次数: 0
摘要
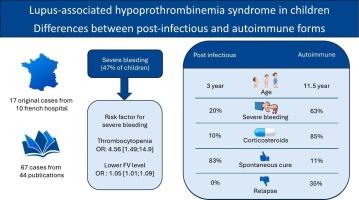
导言狼疮抗凝血功能减退综合征(LAHS)是一种罕见但潜在的严重疾病。LAHS可由感染后(PI)或自身免疫(AI)引起。方法 对法国的病例进行了回顾性多中心研究,随后对文献中的病例进行了回顾。研究共纳入了 84 名患者,其中 17 名患者来自法国队列,67 名患者来自文献系统回顾。95%的患者出现出血性症状,其中近一半病情严重。33%和53%的病例确定有 PI 或 AI 背景。54%的患者接受了皮质类固醇治疗,30%接受了免疫调节治疗。血栓减少症和V因子降低与出血风险升高有关。免疫调节剂组的患儿年龄较大,出血情况明显更严重(p <0.001)。治疗更频繁、更密集,AI 组的复发率更高(p < 0.001)。治疗必须根据临床和生物学背景进行调整。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Lupus-associated hypoprothrombinemia syndrome in children: Differences between post-infectious and autoimmune forms
Introduction
Lupus-anticoagulant hypoprothrombinemia syndrome (LAHS) is a rare but potentially serious condition. LAHS can be of post-infectious (PI) or autoimmune (AI) origin. However, there is currently no clear data available on the differences between these two forms.
Method
A retrospective multicenter study of cases in France was performed, followed by a review of cases in the literature.
Result
A total of 84 patients were included in the study. Seventeen patients were selected from the French cohort, and 67 were selected from a systematic review of the literature. 95 % of patients presented with hemorrhagic symptoms, with nearly half of these cases being severe. PI or AI context was identified in 33 % and 53 % of cases. 54 % of patients were treated with corticosteroids, and 30 % received immunomodulatory therapy. Thrombopenia and lower factor V were associated with a higher risk of bleeding. The AI group consisted of older children and exhibited significantly more severe bleeding (p < 0.001). The treatment was more frequent and intensive, and the relapse rate was higher in the AI group (p < 0.001).
Conclusion
Post-infectious forms are transient and associated with a low risk of serious hemorrhage. The treatment must be adapted according to the clinical and biological context.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Thrombosis research
医学-外周血管病
CiteScore
14.60
自引率
4.00%
发文量
364
审稿时长
31 days
期刊介绍:
Thrombosis Research is an international journal dedicated to the swift dissemination of new information on thrombosis, hemostasis, and vascular biology, aimed at advancing both science and clinical care. The journal publishes peer-reviewed original research, reviews, editorials, opinions, and critiques, covering both basic and clinical studies. Priority is given to research that promises novel approaches in the diagnosis, therapy, prognosis, and prevention of thrombotic and hemorrhagic diseases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


