评估老年手术患者功能障碍的发生率和轨迹:一项观察性队列研究。
IF 5
2区 医学
Q1 ANESTHESIOLOGY
引用次数: 0
摘要
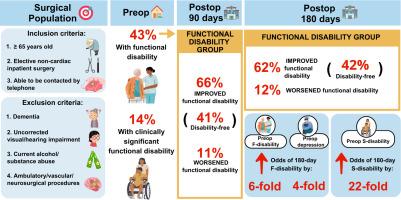
研究目标:目的:(1)估计老年手术患者术前、术后30天、90天和180天时功能障碍超过患者可接受和临床意义水平的发生率和轨迹;(2)确定与术后功能障碍相关的风险因素;(3)比较有功能障碍和无功能障碍参与者的不良临床结局:设计:多中心前瞻性研究:远程术前和术后评估:307名年龄≥65岁接受非心脏手术的老年患者:主要结果:我们发现,133 名(43%)患者在术后出现了严重的功能障碍:我们发现,133 例(43%)患者术前的功能障碍程度超过了患者可接受的水平,其中 42 例(14%)患者的功能障碍程度有临床意义,或至少为中度。与无残疾组相比,功能残疾组的功能改善幅度更大。具体来说,超过 60% 的功能障碍组参与者在术后 90 天和 180 天有明显改善,其中 40% 的人无残疾。然而,12%的功能障碍组和 9%的无残疾组患者在术后 180 天出现了临床意义上的功能障碍恶化。术前功能障碍和抑郁分别与180天后功能障碍几率增加近6倍和4倍有关:结论:与无功能障碍组相比,术前有功能障碍的患者术后功能障碍的改善程度更大。术前功能障碍评估为患者和临床医生的围手术期护理和康复提供了参考。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Evaluating prevalence and trajectory of functional disability in older surgical patients: An observational cohort study
Study objectives
To (1) estimate the prevalence and trajectory of functional disability exceeding patient-acceptable and clinically significant levels in older surgical patients preoperatively and at 30, 90, and 180 days postoperatively, (2) identify risk factors associated with postoperative functional disability, and (3) compare adverse clinical outcomes between participants with and without functional disability.
Design
Multicenter prospective study.
Setting
Remote preoperative and postoperative assessments.
Patients
307 older patients aged ≥65 years undergoing non-cardiac surgery.
Measurements
Functional disability was assessed using the 12-item World Health Organization Disability Assessment Schedule 2.0 on an online survey, with a score ≥ 16 % exceeding a patient-acceptable symptom state and ≥ 35 % indicating significant, or at least moderate, severity.
Main results
We found that 133 (43 %) patients exhibited preoperative functional disability exceeding a patient-acceptable level, with 42 (14 %) experiencing clinically significant, or at least moderate, functional disability. The Functional Disability group showed greater improvement in function than the No-disability group. Specifically, over 60 % of participants in the Functional Disability group showed significant improvement at 90 and 180 days postoperatively, with 40 % being disability-free. However, 12 % of the Functional Disability group and 9 % of the No-disability group experienced a clinically important worsening in functional disability at 180 days postoperatively. Preoperative functional disability and depression were associated with nearly 6- and 4-fold higher odds of functional disability at 180 days, respectively.
Conclusions
Patients with preoperative functional disability experienced greater postoperative improvement in functional disability than the No-disability group. Preoperative evaluation of functional disability informs perioperative care and recovery for patients and clinicians.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
7.40
自引率
4.50%
发文量
346
审稿时长
23 days
期刊介绍:
The Journal of Clinical Anesthesia (JCA) addresses all aspects of anesthesia practice, including anesthetic administration, pharmacokinetics, preoperative and postoperative considerations, coexisting disease and other complicating factors, cost issues, and similar concerns anesthesiologists contend with daily. Exceptionally high standards of presentation and accuracy are maintained.
The core of the journal is original contributions on subjects relevant to clinical practice, and rigorously peer-reviewed. Highly respected international experts have joined together to form the Editorial Board, sharing their years of experience and clinical expertise. Specialized section editors cover the various subspecialties within the field. To keep your practical clinical skills current, the journal bridges the gap between the laboratory and the clinical practice of anesthesiology and critical care to clarify how new insights can improve daily practice.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


