雌激素与乳腺癌
IF 56.7
1区 医学
Q1 ONCOLOGY
引用次数: 0
摘要
雌激素与乳腺癌风险的增加有关。然而,新出现的临床和实验证据表明,孕激素(内源性孕酮或合成孕酮[孕激素])是似乎与雌激素相关的乳腺癌风险的主要激素驱动因素。雌激素可能通过诱导孕酮受体(PR),从而放大孕酮信号,间接导致乳腺癌风险。对激素避孕药的大型研究表明,激素避孕药导致的乳腺癌风险小幅增加主要归因于孕激素,而不是雌激素。雌激素加孕激素的激素替代疗法(HRT)一直显示绝经后妇女患乳腺癌的风险增加,而单独使用雌激素的 HRT 对自然绝经或手术绝经妇女患乳腺癌的风险几乎没有影响。特别是,妇女健康倡议(WHI)随机试验的长期随访表明,单独使用雌激素有好处。最近的数据进一步表明,辅助生殖技术(ART)期间内源性雌激素的升高对乳腺癌风险和复发几乎没有不利影响,甚至有可能降低乳腺癌风险和复发。此外,越来越多的证据表明,抑制孕酮信号传导是抗雌激素降低风险和治疗效果的关键机制。雌激素替代疗法已被证明具有一系列益处,包括改善更年期症状和改善骨骼健康。因此,综合证据表明,雌激素替代疗法可能会给围绝经期或绝经后妇女(包括乳腺癌幸存者)以及为预防卵巢癌而进行预防性输卵管切除术的年轻 BRCA1/2 携带者带来健康益处。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Estrogens and breast cancer
Estrogens have been associated with an increase in breast cancer risk. Yet emerging clinical and experimental evidence points to progestogens [endogenous progesterone or synthetic progesterone (progestin)] as the primary hormonal driver underlying seemingly estrogen-associated breast cancer risk. Estrogens may contribute to breast cancer risk indirectly by induction of the progesterone receptor and thus amplifying progesterone signaling. Large studies of hormonal contraceptives suggest that the small increase in breast cancer risk from hormonal contraceptives is mainly attributable to progestins, not estrogens. Estrogen-plus-progestin hormone replacement therapy (HRT) has consistently shown an increase in breast cancer risk among postmenopausal women, whereas estrogen-alone HRT has little impact on breast cancer risk in naturally or surgically menopausal women. In particular, the long-term follow-up of the Women’s Health Initiative (WHI) randomized trials suggests a benefit of estrogen alone. Recent data further indicate that endogenously elevated estrogen during assisted reproductive technology (ART) exhibits little adverse effect on or potentially a reduction in breast cancer risk and recurrence. Also, accumulating evidence suggests that inhibition of progesterone signaling is a critical mechanism underlying the risk-reducing and therapeutic effects of antiestrogens. Estrogen HRT has shown an array of proven benefits, including ameliorating menopausal symptoms and improving bone health. Collective evidence thus suggests that estrogen HRT is likely to offer health benefits to perimenopausal or postmenopausal women, including breast cancer survivors, as well as young BRCA1/2 carriers with prophylactic oophorectomy for ovarian cancer prevention.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
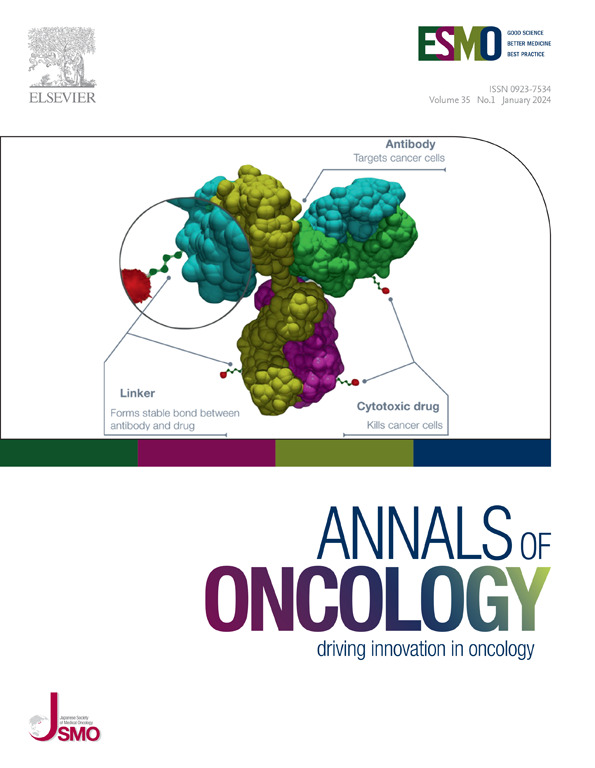
Annals of Oncology
医学-肿瘤学
CiteScore
63.90
自引率
1.00%
发文量
3712
审稿时长
2-3 weeks
期刊介绍:
Annals of Oncology, the official journal of the European Society for Medical Oncology and the Japanese Society of Medical Oncology, offers rapid and efficient peer-reviewed publications on innovative cancer treatments and translational research in oncology and precision medicine.
The journal primarily focuses on areas such as systemic anticancer therapy, with a specific emphasis on molecular targeted agents and new immune therapies. We also welcome randomized trials, including negative results, as well as top-level guidelines. Additionally, we encourage submissions in emerging fields that are crucial to personalized medicine, such as molecular pathology, bioinformatics, modern statistics, and biotechnologies. Manuscripts related to radiotherapy, surgery, and pediatrics will be considered if they demonstrate a clear interaction with any of the aforementioned fields or if they present groundbreaking findings.
Our international editorial board comprises renowned experts who are leaders in their respective fields. Through Annals of Oncology, we strive to provide the most effective communication on the dynamic and ever-evolving global oncology landscape.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


