多发性硬化症患者的合并症及其与预后的关系:快速回顾。
IF 2.9
3区 医学
Q2 CLINICAL NEUROLOGY
引用次数: 0
摘要
导言:多发性硬化症(MS)合并症较多。尽管已知合并症与不良预后之间存在关联,但对个别合并症与残疾、开始治疗和死亡率之间具体关联的全面评估仍然不足。本研究旨在回顾和总结有关合并症与这三种多发性硬化症结果之间关系的现有证据:方法:根据 Cochrane 快速综述方法小组的建议,对 2002 年 1 月至 2023 年 10 月期间的文献进行了快速综述。研究人员检索了 MEDLINE、Embase 和灰色文献,以确定有关合并症对多发性硬化症患者残疾、开始治疗和死亡率影响的研究。对观察性研究和系统性综述分别采用纽卡斯尔-渥太华量表和系统性综述评估工具(AMSTAR-2)标准,系统地进行了数据提取和偏倚风险评估:综述包括 100 项主要研究,涉及 88 种不同的合并症。大多数研究中的女性占 60-80%,研究开始时的平均年龄为 30-45 岁。纳入的研究大多在欧洲、北美和亚洲(特别是中东)进行。半数以上(66%)的特定合并症与结果之间的关系仅在一项研究中进行了探讨,仅有两项研究将开始治疗作为一项结果进行了探讨。用于评估合并症和结果的方法差别很大,包括自我报告测量、医疗记录和诊断代码以及标准化临床评估。抑郁症始终与更严重的残疾(调整后危险比(aHR):1.50-3.59)和死亡率(aHR:1.62-3.55)相关。癫痫同样与残疾程度增加(aOR:1.13-1.77)和死亡率增加(aHR:2.23-3.85)有关。糖尿病一般与死亡率增加有关(aHR:1.39-1.47),但与残疾有关的结果不一致。大多数其他病症仅在一项或两项研究中进行了研究,或者不同研究的结果不尽相同,无法共同表明两者之间存在明确的关联。虽然有 24 项研究对焦虑与残疾的关系进行了评估,但研究结果在可能存在的关联的存在性、方向和强度方面各不相同,需要进行细致的解释:本研究确定了多发性硬化症中各种合并症与三种结果之间的关系,为未来的研究和临床指南奠定了基础。患有精神疾病、代谢疾病和神经系统疾病的人可能会面临更高的多发性硬化症疾病进展风险,因此可能会受益于对其合并症的针对性治疗。总体而言,合并症与多发性硬化症的预后有不同的关联,个别关联需要进一步探讨。不过,有证据表明,某些合并症会导致更严重的残疾和更高的死亡风险,并对开始多发性硬化症治疗造成障碍,因此合并症的预防和管理是多发性硬化症患者护理中不可或缺的一部分:本快速综述的方案已在 PROSPERO 上注册(ID:CRD42023475565),并在 Protocol Exchange (https://doi.org/10.21203/rs.3.pex-2438/v1) 上发布。本文章由计算机程序翻译,如有差异,请以英文原文为准。
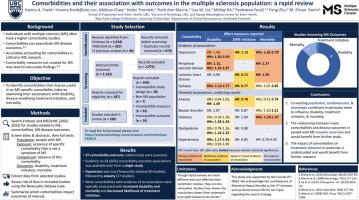
Comorbidities and their association with outcomes in the multiple sclerosis population: A rapid review
Introduction
Multiple sclerosis (MS) has a high comorbidity burden. Despite known associations with adverse outcomes, a comprehensive evaluation of the specific associations between individual comorbidities and disability, treatment initiation, and mortality remains underexplored. This study aimed to review and summarize existing evidence on the association between comorbidities and these three MS outcomes.
Methods
A rapid review spanning the period from January 2002 to October 2023 was conducted following the Cochrane Rapid Review Methods Group recommendations. MEDLINE, Embase, and the grey literature were searched to identify studies examining the effects of comorbidities on disability, treatment initiation, and mortality among individuals with MS. Data extraction and risk of bias assessments were systematically performed, with the Newcastle-Ottawa scale and A MeaSurement Tool to Assess systematic Reviews (AMSTAR-2) criteria for observational studies and systematic reviews respectively.
Results
The review included 100 primary studies, encompassing 88 different comorbidities. Most study populations were between 60–80% female, with an average age of 30–45 years at study start. The majority of included studies were conducted in Europe, North America, and Asia (specifically the Middle East). Over half (66%) of specific comorbidity-outcome relationships were examined within a single study only, and just two studies examined treatment initiation as an outcome. Methods used to assess comorbidities and outcomes varied widely and included self-report measures, medical records and diagnostic codes, and standardized clinical assessments. Depression was consistently associated with greater disability (adjusted hazard ratio (aHR): 1.50–3.59) and mortality (aHR: 1.62–3.55). Epilepsy was similarly associated with increased disability (aOR: 1.13–1.77) and increased mortality (aHR: 2.23–3.85). Diabetes was generally associated with increased mortality (aHR: 1.39–1.47), but results for disability were inconsistent. Most other conditions were examined in one or two studies only or findings varied across studies, unable to collectively indicate a clear association. Although the anxiety-disability relationship was assessed by 24 studies, the findings varied in terms of the presence, direction, and strength of a possible association, requiring nuanced interpretation.
Conclusions
This study identifies relationships between various comorbidities and three outcomes in MS, providing a foundation for future research and clinical guidelines. People with psychiatric, metabolic, and neurological conditions may be at a higher risk of MS disease progression and may therefore benefit from the targeted treatment of their comorbidities. Overall, comorbidities have varying associations with MS outcomes and individual associations require further exploration. However, there is evidence that some comorbidities indicate worse disability and higher mortality risk, and present barriers to initiating MS treatment, making the prevention and management of comorbidities an integral piece of MS patient care.
Protocol
The protocol for this rapid review was registered on PROSPERO (ID: CRD42023475565) and published on Protocol Exchange (https://doi.org/10.21203/rs.3.pex-2438/v1).
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Multiple sclerosis and related disorders
CLINICAL NEUROLOGY-
CiteScore
5.80
自引率
20.00%
发文量
814
审稿时长
66 days
期刊介绍:
Multiple Sclerosis is an area of ever expanding research and escalating publications. Multiple Sclerosis and Related Disorders is a wide ranging international journal supported by key researchers from all neuroscience domains that focus on MS and associated disease of the central nervous system. The primary aim of this new journal is the rapid publication of high quality original research in the field. Important secondary aims will be timely updates and editorials on important scientific and clinical care advances, controversies in the field, and invited opinion articles from current thought leaders on topical issues. One section of the journal will focus on teaching, written to enhance the practice of community and academic neurologists involved in the care of MS patients. Summaries of key articles written for a lay audience will be provided as an on-line resource.
A team of four chief editors is supported by leading section editors who will commission and appraise original and review articles concerning: clinical neurology, neuroimaging, neuropathology, neuroepidemiology, therapeutics, genetics / transcriptomics, experimental models, neuroimmunology, biomarkers, neuropsychology, neurorehabilitation, measurement scales, teaching, neuroethics and lay communication.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


