小儿实体瘤切除术围手术期抗生素的使用:双中心回顾性队列研究
IF 2.4
2区 医学
Q1 PEDIATRICS
引用次数: 0
摘要
目的:关于小儿实体瘤切除术围手术期抗生素的使用尚未达成共识。本研究收集了两家儿科中心的数据,这些中心在儿科实体瘤患者围手术期不同程度地使用了抗生素,以调查术后败血症和感染性并发症的发生情况:方法:这是一项由两家机构共同开展的回顾性队列研究。研究回顾了 2018 年 7 月至 2021 年 6 月间接受实体瘤切除术的儿童病历。分析了手术后 30 天内的患者特征、诊断、手术数据、围手术期抗生素使用情况以及术后感染/败血症。主要结果是术后30天内的手术部位感染(SSI)或全身败血症。进行费雪氏检验以评估差异。结果:2018年7月至2021年6月期间,250名患者在两个中心接受了肿瘤切除术。中位年龄为4岁[范围:0.02-26.1]。75%的患者(N = 188)接受了围手术期抗生素预防(AP),25%的患者未接受AP(N = 62)。使用抗生素组中仅有一名患者(0.5%)出现术后败血症,而未使用抗生素组中有 12 名患者(19.4%)出现败血症(P 结论:使用抗生素组患者的术后败血症发生率低于未使用抗生素组患者:在接受实体瘤切除术的儿童中使用 AP 可降低术后败血症的发生率,但在 SSI 方面没有差异。这可能与手术过程中的细菌转移以及留置中心静脉通路导管的播种有关。我们的研究结果支持在这一人群中标准化使用 AP:回顾性队列研究:证据等级:III。本文章由计算机程序翻译,如有差异,请以英文原文为准。
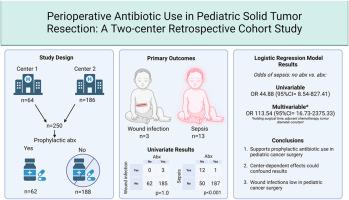
Perioperative Antibiotic Use in Pediatric Solid Tumor Resection: A Two-center Retrospective Cohort Study
Purpose
There is no consensus on the perioperative use of antibiotics in pediatric solid tumor resection. This study collected data from two pediatric centers that utilize perioperative antibiotics to varying degrees in pediatric solid tumor patients to investigate the occurrence of postoperative sepsis and infectious complications.
Methods
A two-institution, retrospective cohort study was performed. Charts of children who underwent solid tumor resection between July 2018–June 2021 were reviewed. Patient characteristics, diagnosis, operative data, perioperative antibiotic use, and postoperative infection/sepsis were analyzed within 30 days of surgery. The primary outcome was surgical site infection (SSI) or systemic sepsis within 30 days of surgery. Fisher's tests were performed to evaluate differences.
Results
250 patients underwent tumor resection between July 2018 and June 2021 at both centers. The median age was 4 years [Range: 0.02–26.1]. Seventy-five percent (N = 188) received perioperative antibiotics prophylaxis (AP), while 25 % of patients did not receive AP (N = 62). Only one patient in the AP group (0.5 %) developed postoperative sepsis, while 12 patients (19.4 %) in the non-AP group developed sepsis (p < 0.0001). There were 3 SSI in the AP group and none in the non-AP group (p = 1.0).
Conclusions
The administration of AP in children undergoing solid tumor resection is associated with a reduced rate of postoperative sepsis but no difference in SSI. This could possibly be related to bacterial translocation during surgery and the seeding of indwelling central venous access catheters. Our results support the standardized use of AP in this population.
Type of Study
Retrospective Cohort Study.
Level of Evidence
III.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
1.10
自引率
12.50%
发文量
569
审稿时长
38 days
期刊介绍:
The journal presents original contributions as well as a complete international abstracts section and other special departments to provide the most current source of information and references in pediatric surgery. The journal is based on the need to improve the surgical care of infants and children, not only through advances in physiology, pathology and surgical techniques, but also by attention to the unique emotional and physical needs of the young patient.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


