FAT家族粘附素的复发性体细胞突变会诱发无性大细胞淋巴瘤的侵袭性表型和不良预后。
IF 6.8
1区 医学
Q1 ONCOLOGY
引用次数: 0
摘要
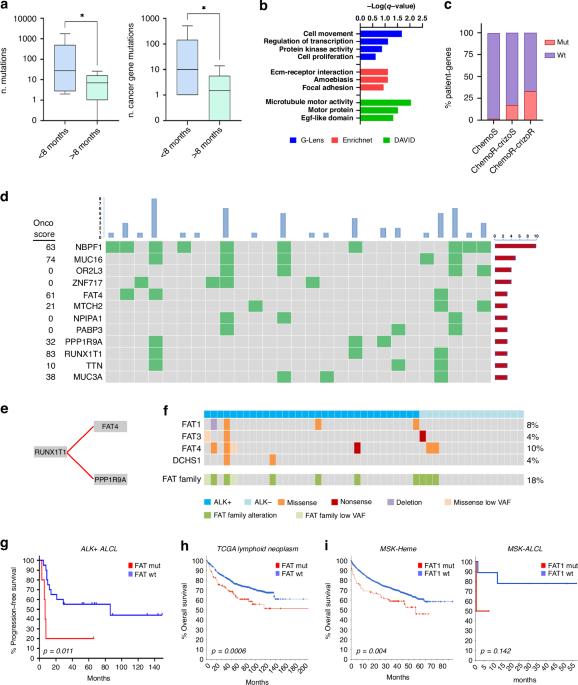
背景:无细胞大细胞淋巴瘤(ALCL)是一种罕见的侵袭性T细胞淋巴瘤,根据涉及ALK基因的染色体易位分为ALK阳性亚型和ALK阴性亚型。目前治疗 ALCL 的标准是多化疗,总生存率较高。然而,一部分患者对这些疗法没有反应或产生耐药性,这给临床医生带来了严峻的挑战。最近的靶向治疗,如ALK激酶抑制剂和抗CD30抗体-药物共轭物已显示出希望,但对一部分患者来说,预后仍不令人满意:我们通过全外显子组测序研究了ALK+ALCL的遗传结构;使用转导的ALCL细胞模型对体外和体内的复发突变进行了表征:结果:发现了FAT家族基因和转录因子RUNX1T1的反复突变。结果:发现了FAT家族基因和转录因子RUNX1T1的反复突变,这些突变诱导了ALCL细胞形态、生长和迁移的变化,揭示了导致耐药性的潜在因素。特别是,ALCL细胞中的FAT4沉默激活了在肿瘤生长中起关键作用的β-catenin和YAP1通路,并导致对化疗的耐药性。此外,STAT1和STAT3在这些细胞中被过度激活。基因表达谱分析显示,与细胞粘附、细胞骨架组织和致癌信号转导相关的通路发生了全面变化。值得注意的是,FAT突变与患者的不良预后有关:这些发现为了解 ALCL 的分子特征提供了新的视角,有助于改善 ALCL 患者的治疗策略和预后。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Recurrent somatic mutations of FAT family cadherins induce an aggressive phenotype and poor prognosis in anaplastic large cell lymphoma
Anaplastic Large Cell Lymphoma (ALCL) is a rare and aggressive T-cell lymphoma, classified into ALK-positive and ALK-negative subtypes, based on the presence of chromosomal translocations involving the ALK gene. The current standard of treatment for ALCL is polychemotherapy, with a high overall survival rate. However, a subset of patients does not respond to or develops resistance to these therapies, posing a serious challenge for clinicians. Recent targeted treatments such as ALK kinase inhibitors and anti-CD30 antibody-drug conjugates have shown promise but, for a fraction of patients, the prognosis is still unsatisfactory. We investigated the genetic landscape of ALK + ALCL by whole-exome sequencing; recurring mutations were characterized in vitro and in vivo using transduced ALCL cellular models. Recurrent mutations in FAT family genes and the transcription factor RUNX1T1 were found. These mutations induced changes in ALCL cells morphology, growth, and migration, shedding light on potential factors contributing to treatment resistance. In particular, FAT4 silencing in ALCL cells activated the β-catenin and YAP1 pathways, which play crucial roles in tumor growth, and conferred resistance to chemotherapy. Furthermore, STAT1 and STAT3 were hyper-activated in these cells. Gene expression profiling showed global changes in pathways related to cell adhesion, cytoskeletal organization, and oncogenic signaling. Notably, FAT mutations associated with poor outcome in patients. These findings provide novel insights into the molecular portrait of ALCL, that could help improve treatment strategies and the prognosis for ALCL patients.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
British Journal of Cancer
医学-肿瘤学
CiteScore
15.10
自引率
1.10%
发文量
383
审稿时长
6 months
期刊介绍:
The British Journal of Cancer is one of the most-cited general cancer journals, publishing significant advances in translational and clinical cancer research.It also publishes high-quality reviews and thought-provoking comment on all aspects of cancer prevention,diagnosis and treatment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


