验证并完善 2022 年欧洲白血病网络(European LeukaemiaNet)对接受异体造血细胞移植的急性髓性白血病患者进行的遗传风险分类
IF 12.8
1区 医学
Q1 HEMATOLOGY
引用次数: 0
摘要
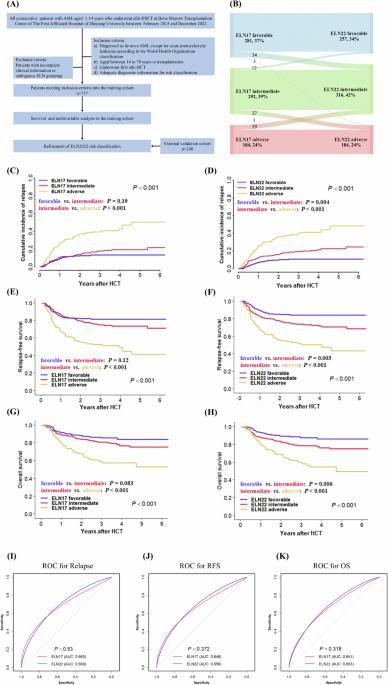
共有757名新生急性髓细胞白血病患者符合培训队列的条件,其中男性401人,女性356人,异体器官移植后的中位随访时间为30个月(1-91个月)。allo-HCT时的中位年龄为40岁(14-69岁)。根据ELN2022分类,34%(n = 257)为良好,42%(n = 316)为中等,24%(n = 180)为不良。与ELN2017的分类相比,ELN2022分类中95%的有利患者、80%的中等患者和84%的不利患者仍处于先前的风险分层中。从ELN2017到ELN2022的患者和主要突变类型的重新分布见图1B和表S1,详细的基线人口统计学数据见表S2。根据ELN2017,有利组、中间组和不利组的3年累积复发率(CIR)分别为13%、18%和40%,相应的无复发生存率(RFS)分别为81%、75%和52%,总生存率(OS)分别为85%、81%和59%,差异均有统计学意义(P <0.001)(图1C、E、G)。在ELN2022中,有利组、中间组和不利组的3年CIR分别为11%、19%和40%(P< 0.001);3年RFS分别为84%、74%和52%(P< 0.001);3年OS分别为88%、79%和59%(P< 0.001)(图1D、F、H)。如果将生存率分析局限于异体肝移植时获得完全缓解(CR)的患者,也能观察到类似的结果(图 S1)。此外,在多变量模型中,诊断时的ELN2022风险分类是CIR、RFS和OS的独立预后因素(表S3)。为了比较ELN2022和ELN2017风险系统在我们的训练队列中的预后预测能力,我们进行了接收者操作特征(ROC)分析。预测复发(AUCELN2017 = 0.660 vs. AUCELN2022 = 0.668,P = 0.530)、RFS(AUCELN2017 = 0.648 vs. AUCELN2022 = 0.658,P = 0.372)和 OS(AUCELN2017 = 0.641 vs. AUCELN2022 = 0.653,P = 0.318)在 ELN2022 和 ELN2017 之间无明显差异(图 1I-K 和表 S4)。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Validation and refinement of the 2022 European LeukaemiaNet genetic risk classification of acute myeloid leukaemia patients receiving allogeneic haematopoietic cell transplantation
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Leukemia
医学-血液学
CiteScore
18.10
自引率
3.50%
发文量
270
审稿时长
3-6 weeks
期刊介绍:
Title: Leukemia
Journal Overview:
Publishes high-quality, peer-reviewed research
Covers all aspects of research and treatment of leukemia and allied diseases
Includes studies of normal hemopoiesis due to comparative relevance
Topics of Interest:
Oncogenes
Growth factors
Stem cells
Leukemia genomics
Cell cycle
Signal transduction
Molecular targets for therapy
And more
Content Types:
Original research articles
Reviews
Letters
Correspondence
Comments elaborating on significant advances and covering topical issues
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


