Cimicifuga heracleifolia kom.通过 PI3K/AKT/NF-κB 信号通路减轻溃疡性结肠炎。
IF 4.8
2区 医学
Q1 CHEMISTRY, MEDICINAL
引用次数: 0
摘要
民族药理学的相关性:Cimicifuga heracleifolia Kom.(C. heracleifolia)在治疗胃肠道疾病(包括脾虚性腹泻)方面具有显著疗效。溃疡性结肠炎(UC)是一种慢性炎症性肠病,与脾虚性腹泻有相似之处。然而,C. heracleifolia 对溃疡性结肠炎的药理作用及其潜在机制仍有待探索:本研究探讨了C. heracleifolia对UC的治疗潜力和机制:方法:首先,采用网络药理学分析,包括成分筛选、靶点预测、蛋白质-蛋白质相互作用(PPI)网络分析和富集分析,来预测C. heracleifolia的作用机制。在葡聚糖硫酸钠(DSS)诱导的 UC 模型中,利用转录组学和功能测定进一步验证了研究结果。此外,还通过表面等离子体共振(SPR)分析、分子对接和基于细胞的检测鉴定了生物活性化合物:结果:共筛选出 52 种 C. heracleifolia 成分,并在由 285 个潜在治疗靶点组成的 PPI 网络中确定了 32 个关键靶点。富集分析表明,C. heracleifolia的抗UC作用是通过调节免疫反应和抑制炎症信号通路介导的。体内实验表明,C. heracleifolia减轻了结肠的组织学损伤,降低了磷酸化Akt1、核因子-kappa B(NF-κB)p65和Kappa B激酶α/β抑制剂(IKKα/β)的表达,抑制了白细胞介素-1β(IL-1β)、白细胞介素-6(IL-6)和肿瘤坏死因子-α(TNF-α)的含量,并增强了紧密连接蛋白的表达。此外,cimigenoside、咖啡酸和咖啡酸甲酯被鉴定为导致 C. heracleifolia 治疗 UC 效果的生物活性成分:总之,本研究首次证明了 C. heracleifolia 通过增强肠粘膜屏障和抑制磷脂酰肌醇 3- 激酶(PI3K)/AKT/NF-κB 信号通路对 UC 发挥治疗作用。这些发现为 C. heracleifolia 在治疗 UC 方面的临床应用提供了宝贵的见解。本文章由计算机程序翻译,如有差异,请以英文原文为准。
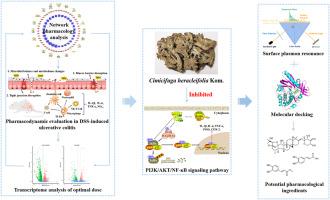
Cimicifuga heracleifolia kom. Attenuates ulcerative colitis through the PI3K/AKT/NF-κB signaling pathway
Ethnopharmacological relevance
Cimicifuga heracleifolia Kom. (C. heracleifolia) has demonstrated efficacy in treating gastrointestinal disorders, including splenasthenic diarrhea. Ulcerative colitis (UC), a chronic inflammatory bowel disease, shares similarities with splenasthenic diarrhea. However, the pharmacological effects of C. heracleifolia on UC and the underlying mechanisms remain unexplored.
Aim of the study
The present study investigates the therapeutic potential and mechanisms of C. heracleifolia in UC.
Methods
Initially, network pharmacology analysis, encompassing ingredient screening, target prediction, protein-protein interaction (PPI) network analysis, and enrichment analysis, was employed to predict the mechanisms of C. heracleifolia. The findings were further validated using transcriptomics and functional assays in a dextran sulfate sodium (DSS)-induced UC model. Additionally, bioactive compounds were identified through surface plasmon resonance (SPR) analysis, molecular docking, and cell-based assays.
Results
A total of 52 ingredients of C. heracleifolia were screened, and 32 key targets were identified within a PPI network comprising 285 potential therapeutic targets. Enrichment analysis indicated that the anti-UC effects of C. heracleifolia are mediated through immune response modulation and the inhibition of inflammatory signaling pathways. In vivo experiments showed that C. heracleifolia mitigated histological damage in the colon, reduced the expression of phosphorylated Akt1, nuclear factor-kappa B (NF-κB) p65, and inhibitor of Kappa B kinase α/β (IKKα/β), suppressed the content of interleukin-1β (IL-1β), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α), and enhanced the expression of tight junction proteins. Moreover, cimigenoside, caffeic acid, and methyl caffeate were identified as the bioactive constituents responsible for the UC treatment effects of C. heracleifolia.
Conclusions
In summary, this study is the first to demonstrate that C. heracleifolia exerts therapeutic effects on UC by enhancing the intestinal mucosal barrier and inhibiting the phosphatidylinositol 3-kinase (PI3K)/AKT/NF-κB signaling pathway. These findings offer valuable insights into the clinical application of C. heracleifolia for UC management.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Journal of ethnopharmacology
医学-全科医学与补充医学
CiteScore
10.30
自引率
5.60%
发文量
967
审稿时长
77 days
期刊介绍:
The Journal of Ethnopharmacology is dedicated to the exchange of information and understandings about people''s use of plants, fungi, animals, microorganisms and minerals and their biological and pharmacological effects based on the principles established through international conventions. Early people confronted with illness and disease, discovered a wealth of useful therapeutic agents in the plant and animal kingdoms. The empirical knowledge of these medicinal substances and their toxic potential was passed on by oral tradition and sometimes recorded in herbals and other texts on materia medica. Many valuable drugs of today (e.g., atropine, ephedrine, tubocurarine, digoxin, reserpine) came into use through the study of indigenous remedies. Chemists continue to use plant-derived drugs (e.g., morphine, taxol, physostigmine, quinidine, emetine) as prototypes in their attempts to develop more effective and less toxic medicinals.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


