2 型糖尿病患者线粒体肌酸激酶 2 减少会损害骨骼肌线粒体功能,与胰岛素无关。
IF 15.8
1区 医学
Q1 CELL BIOLOGY
引用次数: 0
摘要
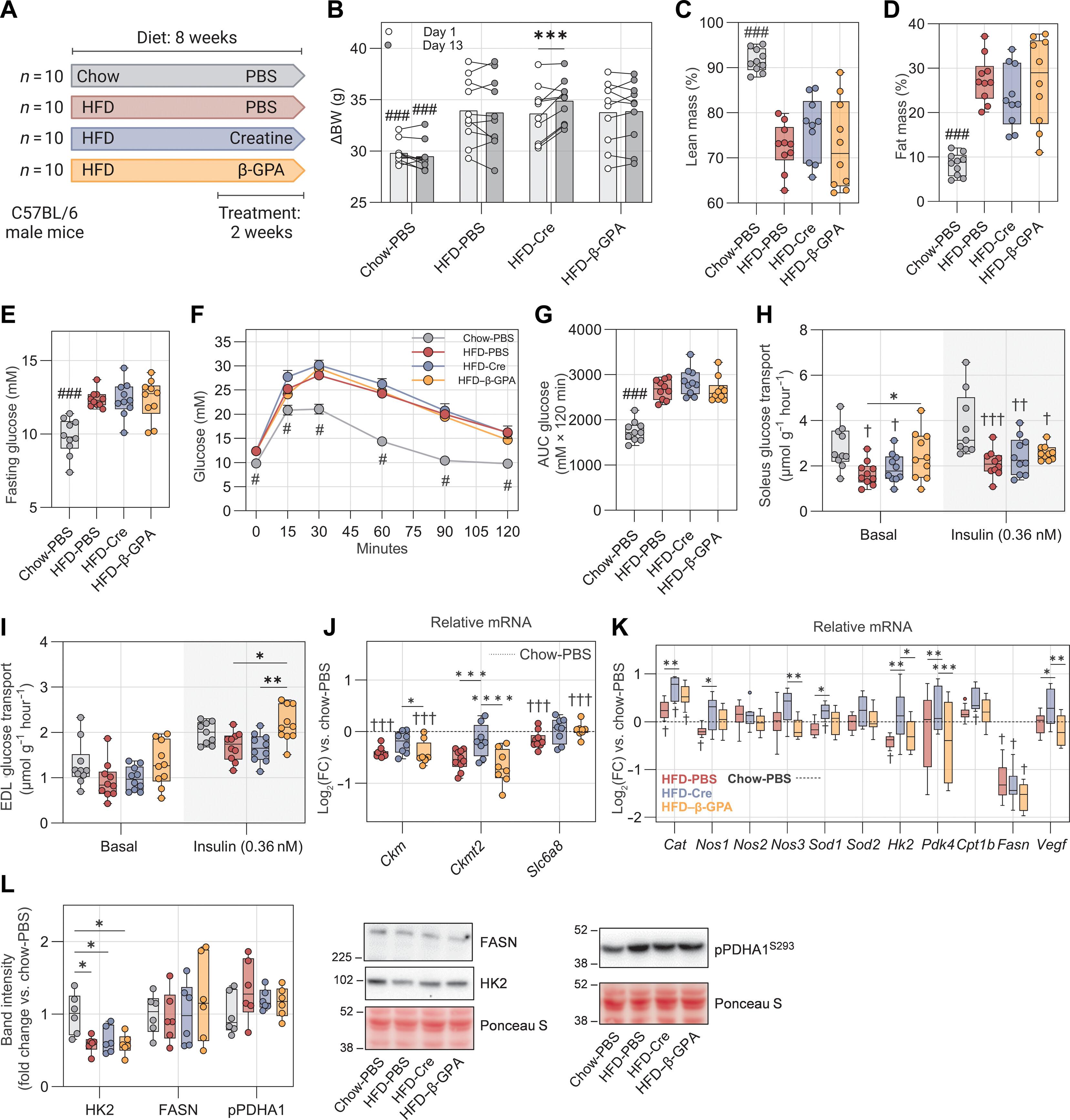
血浆肌酸浓度的升高与罹患 2 型糖尿病的风险有关,但这种变化是否与新陈代谢障碍有关或因果关系仍有待探讨。由于骨骼肌是肌酸和葡萄糖的主要排泄场所,我们研究了肌肉内肌酸代谢在 2 型糖尿病胰岛素抵抗的病理生理学中的作用。在患有 2 型糖尿病的男性中,血浆肌酸浓度升高,肌肉内磷酸肌酸含量降低。这些变化与肉瘤线粒体肌酸激酶 2(CKMT2)的表达减少有关。在以高脂饮食喂养的 C57BL/6 小鼠中,连续 2 周补充肌酸或连续 1 周使用肌酸类似物 β-GPA 都不会引起葡萄糖耐量的变化,这表明循环中肌酸的增加与胰岛素抵抗有关,而不是导致胰岛素抵抗。在 C2C12 肌细胞管中,使用小干扰 RNA 沉默 Ckmt2 可降低线粒体呼吸、膜电位和葡萄糖氧化。电穿孔介导的 Ckmt2 在高脂饮食喂养的雄性小鼠骨骼肌中的过表达增加了线粒体呼吸,这与肌酸的可用性无关。鉴于 Ckmt2 的过表达能改善线粒体功能,我们探讨了运动是否能调节 CKMT2 的表达。对公开数据的分析表明,人和小鼠的 CKMT2 含量都会因运动训练而上调。我们揭示了 CKMT2 在线粒体稳态中除了肌酸磷酸化的功能外,还在胰岛素作用之外发挥了以前未被重视的作用。总之,我们的数据为 CKMT2 如何介导与 2 型糖尿病相关的线粒体功能障碍提供了功能性证据。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Decreased mitochondrial creatine kinase 2 impairs skeletal muscle mitochondrial function independently of insulin in type 2 diabetes
Increased plasma creatine concentrations are associated with the risk of type 2 diabetes, but whether this alteration is associated with or causal for impairments in metabolism remains unexplored. Because skeletal muscle is the main disposal site of both creatine and glucose, we investigated the role of intramuscular creatine metabolism in the pathophysiology of insulin resistance in type 2 diabetes. In men with type 2 diabetes, plasma creatine concentrations were increased, and intramuscular phosphocreatine content was reduced. These alterations were coupled to reduced expression of sarcomeric mitochondrial creatine kinase 2 (CKMT2). In C57BL/6 mice fed a high-fat diet, neither supplementation with creatine for 2 weeks nor treatment with the creatine analog β-GPA for 1 week induced changes in glucose tolerance, suggesting that increased circulating creatine was associated with insulin resistance rather than causing it. In C2C12 myotubes, silencing Ckmt2 using small interfering RNA reduced mitochondrial respiration, membrane potential, and glucose oxidation. Electroporation-mediated overexpression of Ckmt2 in skeletal muscle of high-fat diet–fed male mice increased mitochondrial respiration, independent of creatine availability. Given that overexpression of Ckmt2 improved mitochondrial function, we explored whether exercise regulates CKMT2 expression. Analysis of public data revealed that CKMT2 content was up-regulated by exercise training in both humans and mice. We reveal a previously underappreciated role of CKMT2 in mitochondrial homeostasis beyond its function for creatine phosphorylation, independent of insulin action. Collectively, our data provide functional evidence for how CKMT2 mediates mitochondrial dysfunction associated with type 2 diabetes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Science Translational Medicine
CELL BIOLOGY-MEDICINE, RESEARCH & EXPERIMENTAL
CiteScore
26.70
自引率
1.20%
发文量
309
审稿时长
1.7 months
期刊介绍:
Science Translational Medicine is an online journal that focuses on publishing research at the intersection of science, engineering, and medicine. The goal of the journal is to promote human health by providing a platform for researchers from various disciplines to communicate their latest advancements in biomedical, translational, and clinical research.
The journal aims to address the slow translation of scientific knowledge into effective treatments and health measures. It publishes articles that fill the knowledge gaps between preclinical research and medical applications, with a focus on accelerating the translation of knowledge into new ways of preventing, diagnosing, and treating human diseases.
The scope of Science Translational Medicine includes various areas such as cardiovascular disease, immunology/vaccines, metabolism/diabetes/obesity, neuroscience/neurology/psychiatry, cancer, infectious diseases, policy, behavior, bioengineering, chemical genomics/drug discovery, imaging, applied physical sciences, medical nanotechnology, drug delivery, biomarkers, gene therapy/regenerative medicine, toxicology and pharmacokinetics, data mining, cell culture, animal and human studies, medical informatics, and other interdisciplinary approaches to medicine.
The target audience of the journal includes researchers and management in academia, government, and the biotechnology and pharmaceutical industries. It is also relevant to physician scientists, regulators, policy makers, investors, business developers, and funding agencies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


