下腔静脉造影剂反流等级与急性肺栓塞的心脏指数降低有关。
IF 3.7
3区 医学
Q1 HEMATOLOGY
引用次数: 0
摘要
背景和目的:中危肺栓塞(PE)患者通常会出现心脏指数(CI)明显降低的情况。然而,识别这种更严重的情况需要有创血液动力学监测。下腔静脉(IVC)造影剂反流作为右心室功能恶化的标志,是否能预测有创血流动力学尚未进行探讨:这是一项为期 3 年的单中心回顾性研究,研究对象是接受机械血栓切除术并同时接受肺动脉导管检查的连续 PE 患者。对 CT 肺血管造影进行复查,并根据既定标准将造影剂反流分为无/轻微反流(仅限于 IVC)或大量反流(包括肝静脉的不透明):85 例患者中有 29 例(34%)存在大量造影剂回流,且与较低的 CI 有关(1.8 ± 0.4 L/min/m2 v. 2.6 ± 1.0 L/min/m2,P 3),CI ≤2.2 L/min/m2 的显著预测因子(OR:22.5,95 % CI:4.8,104.4,P 2 分别为 62.6%、93.1%、94.6% 和 56.2%)。这些结果在多变量模型中仍有意义,在分离中危患者(n = 72,85%)时也类似:结论:造影剂反流程度对 PE 患者心脏指数降低具有高度特异性,即使将中危患者分离出来也是如此。实时预测血液动力学特征可能会为 PE 的风险分级带来更多价值。本文章由计算机程序翻译,如有差异,请以英文原文为准。
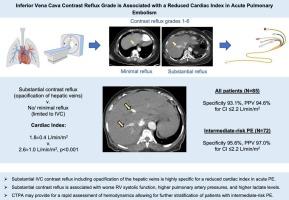
Inferior vena cava contrast reflux grade is associated with a reduced cardiac index in acute pulmonary embolism
Background and Aims
Patients with intermediate-risk pulmonary embolism (PE) commonly present with a significantly reduced cardiac index (CI). However, the identification of this more severe profile requires invasive hemodynamic monitoring. Whether inferior vena cava (IVC) contrast reflux, as a marker of worse right ventricular function, can predict invasive hemodynamics has not been explored.
Methods
This was a single-center retrospective study over a 3-year period of consecutive patients with PE undergoing mechanical thrombectomy and simultaneous pulmonary artery catheterization. CT pulmonary angiograms were reviewed, and contrast reflux was graded as no/minimal reflux (limited to the IVC) or substantial (opacification including hepatic veins) based on an established scale.
Results
Substantial contrast reflux was present in 29 of 85 patients (34 %) and associated with a lower CI (1.8 ± 0.4 L/min/m2 v. 2.6 ± 1.0 L/min/m2, p < 0.001), higher pulmonary artery systolic pressure (53.2 ± 19.5 mmHg v. 44.0 ± 12.1 mmHg, p = 0.025), and worse right ventricular systolic function. An IVC contrast reflux grade > 3 was a significant predictor for a CI ≤2.2 L/min/m2 (OR: 22.5, 95 % CI: 4.8, 104.4, p < 0.001). Sensitivity, specificity, positive predictive value, and negative predictive value for substantial contrast reflux for a CI ≤2.2 L/min/m2 were 62.6 %, 93.1 %, 94.6 %, and 56.2 %, respectively. These findings remained significant in a multivariable model and were similar when isolating for intermediate-risk patients (n = 72, 85 %).
Conclusions
The degree of contrast reflux is highly specific for a reduced cardiac index in PE even when isolating for intermediate-risk patients. Real-time prediction of a hemodynamic profile may have added value in the risk-stratification of PE.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Thrombosis research
医学-外周血管病
CiteScore
14.60
自引率
4.00%
发文量
364
审稿时长
31 days
期刊介绍:
Thrombosis Research is an international journal dedicated to the swift dissemination of new information on thrombosis, hemostasis, and vascular biology, aimed at advancing both science and clinical care. The journal publishes peer-reviewed original research, reviews, editorials, opinions, and critiques, covering both basic and clinical studies. Priority is given to research that promises novel approaches in the diagnosis, therapy, prognosis, and prevention of thrombotic and hemorrhagic diseases.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


