代谢性肥胖表型与总体癌症和特定部位癌症风险的关系:队列研究的系统回顾和荟萃分析。
IF 6.4
1区 医学
Q1 ONCOLOGY
引用次数: 0
摘要
背景:众所周知,肥胖是某些癌症的风险因素之一;然而,对于肥胖程度高但代谢健康状况不同的人患癌症的风险是否存在差异,目前尚不清楚。本系统性文献综述和队列研究荟萃分析旨在评估代谢性肥胖表型与总体和特定部位癌症风险之间的关联:方法:使用PubMed和Embase数据库确定截至2023年6月6日的相关队列研究。采用随机效应模型估算代谢性肥胖表型与癌症风险之间关系的汇总相对风险(SRR)和95%置信区间(CI)。采用 Cochrane 方法和 GRADE 工具对证据的确定性进行了评估。本研究已在 PROSPERO 注册,编号为 CRD42024549511:本研究共筛选了 15,556 条记录,并纳入了涵盖 15 项队列研究的 31 篇出版物。在这些研究中,22 项被评估为存在低偏倚风险,9 项存在中度偏倚风险。与代谢健康的正常体重者(MHNW)相比,代谢不健康的超重/肥胖者(MUOW/OB)罹患总体癌症(SRR = 1.21,95% CI = 1.02-1.44,n = 3 项研究,高确定性)和肥胖相关癌症(SRR = 1.42,95% CI = 1.15-1.74,n = 3,极低确定性)的风险更高。具体而言,MUOW/OB 患者罹患绝经后乳腺癌(SRR = 1.32,95% CI = 1.17-1.48,n = 7,低确定性)、结肠直肠癌(SRR = 1.24,95% CI = 1.16-1.31,n = 6,中确定性)和肥胖相关癌症(SRR = 1.42,95% CI = 1.15-1.74,n = 3,极低确定性)的风险较高。31,n = 6,中等确定性)、子宫内膜(SRR = 2.31,95% CI = 2.08-2.57,n = 4,高度确定性)、甲状腺(SRR = 1.42,95% CI = 1.29-1.57,n = 4,中等确定性)、肾脏(SRR = 1.71,95% CI = 1.40-2.10,n = 3,低度确定性)、胰腺(SRR = 1.35,95% CI = 1.24-1.47,n = 3,高度确定性)、肝脏(SRR = 1.81,95% CI = 1.36-2.42,n = 2,中度确定性)、胆囊(SRR = 1.42,95% CI = 1.17-1.73,n = 2,高度确定性)、膀胱(SRR = 1.36,95% CI = 1.19-1.56,n = 2,中度确定性)和胃(SRR = 1.50,95% CI = 1.12-2.01,n = 2,高度确定性)。此外,我们还发现,与表型为 MHNW 的人相比,表型为 MUNW 和 MHOW/OB 的人罹患大多数癌症的风险更高。我们根据代谢性肥胖表型进行的分层分析表明,MUOW/OB表型的人患某些癌症的风险高于MHOW/OB或MUNW表型的人:这些研究结果表明,较高的脂肪含量和代谢功能障碍都与几种癌症风险的增加有独立的关联,而在同时患有代谢功能障碍和肥胖症的人群中观察到的关联性最强。本文章由计算机程序翻译,如有差异,请以英文原文为准。
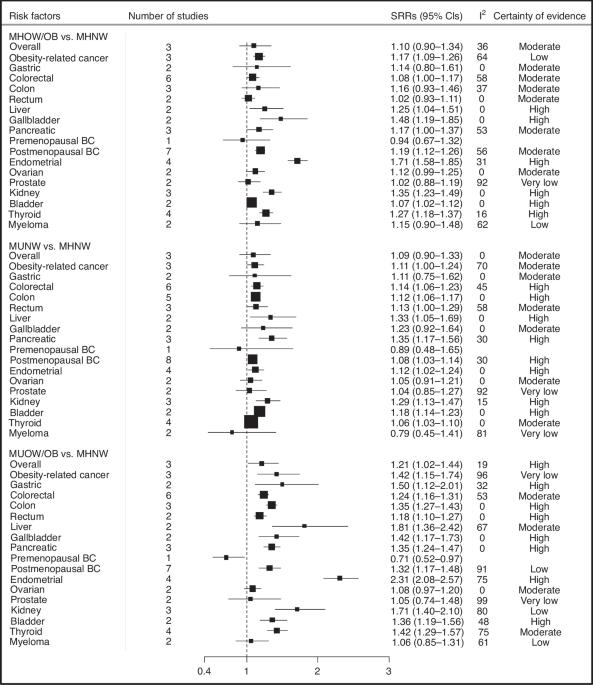
Association of metabolic obesity phenotypes with risk of overall and site-specific cancers: a systematic review and meta-analysis of cohort studies
Adiposity is a known risk factor for certain cancers; however, it is not clear whether the risk of cancer differs between individuals with high adiposity but different metabolic health status. The aim of this systematic literature review and meta-analysis of cohort studies was to evaluate associations between metabolic obesity phenotypes and overall and site-specific cancer risk. PubMed and Embase databases were used to identify relevant cohort studies up to the 6th of June 2023. Random-effects models were used to estimate summary relative risks (SRRs) and 95% confidence intervals (CIs) for the association between metabolic obesity phenotypes and cancer risk. Certainty of evidence was assessed using the Cochrane methods and the GRADE tool. This study is registered with PROSPERO, number CRD42024549511. A total of 15,556 records were screened, and 31 publications covering 15 unique cohort studies were included in this analysis. Of these studies, 22 were evaluated as being at low risk of bias and 9 at moderate risk of bias. Compared to metabolically healthy normal-weight individuals (MHNW), metabolically unhealthy overweight/obese (MUOW/OB) individuals had a higher risk of overall (SRR = 1.21, 95% CI = 1.02–1.44, n = 3 studies, high certainty) and obesity-related cancers (SRR = 1.42, 95% CI = 1.15–1.74, n = 3, very low certainty). Specifically, MUOW/OB individuals were at higher risk of cancers of the postmenopausal breast (SRR = 1.32, 95% CI = 1.17–1.48, n = 7, low certainty), colorectum (SRR = 1.24, 95% CI = 1.16–1.31, n = 6, moderate certainty), endometrium (SRR = 2.31, 95% CI = 2.08–2.57, n = 4, high certainty), thyroid (SRR = 1.42, 95% CI = 1.29–1.57, n = 4, moderate certainty), kidney (SRR = 1.71, 95% CI = 1.40–2.10, n = 3, low certainty), pancreas (SRR = 1.35, 95% CI = 1.24–1.47, n = 3, high certainty), liver (SRR = 1.81, 95% CI = 1.36–2.42, n = 2, moderate certainty), gallbladder (SRR = 1.42, 95% CI = 1.17–1.73, n = 2, high certainty), bladder (SRR = 1.36, 95% CI = 1.19–1.56, n = 2, moderate certainty), and stomach (SRR = 1.50, 95% CI = 1.12–2.01, n = 2, high certainty). In addition, we found elevated risks of most of these cancers among individuals classified as MUNW and MHOW/OB phenotypes compared to those with MHNW phenotype. Our stratified analyses according to metabolic obesity phenotypes suggested that the elevated risks of some cancers were stronger in individuals with MUOW/OB versus those with MHOW/OB or MUNW phenotypes. These findings suggest that both higher adiposity and metabolic dysfunction were independently associated with increased risk of several cancers, with the strongest associations generally observed among those with both metabolic dysfunction and obesity.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
British Journal of Cancer
医学-肿瘤学
CiteScore
15.10
自引率
1.10%
发文量
383
审稿时长
6 months
期刊介绍:
The British Journal of Cancer is one of the most-cited general cancer journals, publishing significant advances in translational and clinical cancer research.It also publishes high-quality reviews and thought-provoking comment on all aspects of cancer prevention,diagnosis and treatment.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


