使用无对比定量磁共振成像技术进行保肝立体定向烧蚀体放射治疗的可行性
IF 2.7
3区 医学
Q3 ONCOLOGY
引用次数: 0
摘要
背景和目的肝脏肿瘤通常是在肝硬化和肝功能受损的背景下发生的。因此,放射治疗受到辐射诱发肝病的限制,其参数为肝脏平均剂量(LMD)。肝功能是高度异质性的,尤其是在肝癌患者中,但使用 LMD 并没有考虑到这一点。改善肝脏治疗的一个可行方法是使用定量成像技术评估肝脏健康状况,并优先保留健康的肝脏组织。材料与方法为 10 名肝脏转移患者提供了解剖 T2 和定量铁校正 T1 (cT1) 图像。在定量图像上使用阈值自动分割功能性肝脏体积。肝脏立体定向消融体放射治疗(SABR)计划是根据科室协议制定的。结果疏肝计划实现了肝脏功能性平均剂量的显著降低(P=0.002),平均降低1.4 Gy。LMD也有显著差异(P=0.002),但幅度较小,平均减少0.7 Gy。规划靶体积D99%存在一些差异(p=0.04),但疏导计划仍在最佳容差范围内,D95%也无明显差异(p=0.2)。结论这项研究首次证明了cT1地图在放疗中的应用,显示对健康肝脏的剂量显著减少。还需要进一步在肝癌患者中进行验证,因为肝癌患者可能受益最大。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Feasibility of using contrast-free quantitative magnetic resonance imaging for liver sparing stereotactic ablative body radiotherapy
Background and purpose
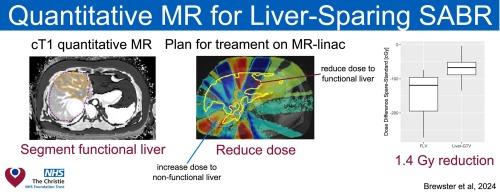
Tumours in the liver often develop on a background of liver cirrhosis and impaired liver function. As a result, radiotherapy treatments are limited by radiation-induced liver disease, parameterised by the liver mean dose (LMD). Liver function is highly heterogeneous, especially in liver cancer, but the use of LMD does not take this into account. One possible way to improve liver treatments is to use quantitative imaging techniques to assess liver health and prioritise the sparing of healthy liver tissue.
Materials and methods
Anatomical T2 and quantitative iron-corrected T1 (cT1) images were made available for 10 patients with liver metastases. Functional liver volumes were automatically segmented on the quantitative images using a threshold. Liver stereotactic ablative body radiotherapy (SABR) plans were made using a departmental protocol. Liver-sparing plans were then made by reducing the dose to the functional sub-volume.
Results
The sparing plans achieved a statistically significant () reduction in the functional liver mean dose, with a mean reduction of 1.4 Gy. The LMD was also significantly different () but had a smaller magnitude with a mean reduction of 0.7 Gy. There were some differences in the planning target volume D99% () but the sparing plans remained within the optimal tolerance and the D95% was not significantly different ().
Conclusions
This study has, for the first time, demonstrated the use of cT1 maps in radiotherapy showing significant reductions in dose to the healthy liver. Further work is needed to validate this in liver cancer patients, who would likely benefit most.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Clinical and Translational Radiation Oncology
Medicine-Radiology, Nuclear Medicine and Imaging
CiteScore
5.30
自引率
3.20%
发文量
114
审稿时长
40 days
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


