并发 MASLD 的慢性乙型肝炎患者出现明显纤维化的患病率和风险因素。
IF 3.7
3区 医学
Q2 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
引言和目的:显著纤维化是慢性乙型肝炎(CHB)和代谢功能障碍相关性脂肪性肝病(MASLD)临床干预的指标。关于活组织检查确定的 MASLD 对慢性乙型肝炎患者显著纤维化的临床影响的数据仍然很少。目前的研究旨在阐明伴有MASLD的CHB患者发生明显纤维化的风险是否更高:这项在两家三甲医院进行的回顾性研究包括2009年至2021年间1818例未接受抗病毒治疗的CHB和肝脂肪变性患者。CHB组(n=844)和CHB+MASLD组(n=974)的肝活检病理结果进行了对比。METAVIR的F≥2值用于对明显纤维化进行分类:结果:CHB + MASLD 患者的纤维化程度更高(35.5% vs. 23.5%,p):MASLD与CHB患者较高的纤维化分期有关。对于有三个或三个以上心脏代谢风险因素的患者来说,早期发现和干预至关重要。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Prevalence and risk factors of significant fibrosis in chronic hepatitis B patients with concurrent metabolic dysfunction-associated steatotic liver disease
Introduction and objectives
Significant fibrosis is an indicator of clinical intervention for both chronic hepatitis B (CHB) and metabolic dysfunction-associated steatotic liver disease (MASLD). There remains a paucity of data regarding the clinical impact of biopsy-defined MASLD on significant fibrosis in CHB patients. The current study aims to elucidate whether patients with concomitant MASLD are at higher risk of significant fibrosis in patients with CHB.
Patients and methods
This retrospective research of two tertiary hospitals comprised 1818 patients between 2009 and 2021 with CHB and hepatic steatosis who had not received antiviral therapy. Pathologic findings by liver biopsy were contrasted between CHB group (n = 844) and CHB + MASLD (n = 974) group. METAVIR values of F≥2 were used to categorize significant fibrosis.
Results
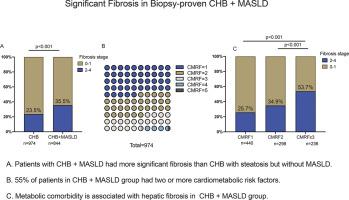
Patients with CHB + MASLD had more significant fibrosis (35.5 % vs. 23.5 %, p < 0.001) than CHB group. The presence of MASLD [adjusted odds ratio (aOR) 2.055, 95 % confidence interval (CI) 1.635–2.584; p < 0.001] was strongly associated with significant fibrosis in all CHB patients. There was a trend for patients with more cardiometabolic risk factors (CMRFs) to have a higher prevalence of significant fibrosis: (25.7 % in CMRF1 subgroup v.s. 34.9 % in CMRF2 subgroup v.s. 53.7 % in CMRF≥ 3 subgroup, p < 0.001). Patients with CMRF≥3 had a three-fold higher significant fibrosis than those with just one CMRF.
Conclusions
MASLD was associated with higher fibrosis stage in patients with CHB. Early detection and intervention are crucial to patients with three or more cardiometabolic risk factors.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Annals of hepatology
医学-胃肠肝病学
CiteScore
7.90
自引率
2.60%
发文量
183
审稿时长
4-8 weeks
期刊介绍:
Annals of Hepatology publishes original research on the biology and diseases of the liver in both humans and experimental models. Contributions may be submitted as regular articles. The journal also publishes concise reviews of both basic and clinical topics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


