肾素血管紧张素系统抑制剂与塔克次氏综合征患者的预后:GEIST 登记的倾向得分分析。
IF 3.7
2区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
引用次数: 0
摘要
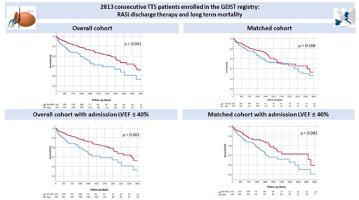
背景关于塔克次氏综合征(TTS)后长期药物治疗及其潜在预后影响的数据很少。本研究旨在评估服用肾素血管紧张素系统抑制剂(RASi)的 TTS 患者的临床特征和长期预后。中位随访时间为 31 个月(四分位距为 12-56 个月)。RASi治疗与未治疗患者的比较在总体人群中进行,并根据年龄、性别、合并症、触发类型和院内并发症进行1:1倾向评分匹配。REGISTRATIONclinicaltrials.gov, NCT04361994, https://clinicaltrials.gov/study/NCT04361994 结果:在2453名活着出院的TTS患者中,1683人(68%)接受了RASi治疗。接受RASi治疗的患者年龄较大(71±11岁 vs 69±13岁,P=0.01),高血压(74% vs 53%,P<0.01)和糖尿病(19% vs 15%,P=0.01)患病率较高,入院左室射血分数(LVEF)较高(41±11% vs 39±12%,P<0.01),院内并发症发生率较低(18.9% vs 29.6%,P<0.01)。在多变量分析中,出院时接受 RASi 治疗与较低的死亡率独立相关(HR 0.63,95%CI 0.45-0.87,p<0.01)。生存分析表明,从长期来看,接受RASi治疗的患者在整个队列中的死亡率较低(对数秩P=0.001)。然而,在配对队列中,接受 RASi 治疗的患者并没有发现这种益处(对数秩 P=0.168)。在总体队列和匹配队列中,RASi的潜在生存获益存在于两个亚组:入院时LVEF≤40%的患者(HR 0.54,95%CI 0.38-0.78,p=0.001;HR 0.59,95%CI 0.37-0.95,p=0.030)和糖尿病(HR 0.41,95%CI 0.23-0.73,p= 0.002;HR 0.41,95%CI 0.21-0.82,p=0.011)。结论TTS发作后长期使用RASi治疗与倾向评分分析中较低的死亡率无关。然而,入院时 LVEF ≤40% 或患有糖尿病的患者可能会获得生存益处。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Renin angiotensin system inhibitors and outcome in patients with takotsubo syndrome: A propensity score analysis of the GEIST registry
Background
Few data are available on long-term drug therapy and its potential prognostic impact after Takotsubo syndrome (TTS). Aim of the study is to evaluate clinical characteristics and long-term outcome of TTS patients on Renin Angiotensin system inhibitors (RASi).
Methods
TTS patients were enrolled in the international multicenter GEIST (GErman Italian Spanish Takotsubo) registry. Median follow-up was 31 (Interquartile range 12-56) months. Comparison of RASi treated vs. untreated patients was performed within the overall population and after 1:1 propensity score matching for age, sex, comorbidities, type of trigger and in-hospital complications.
Registration
clinicaltrials.gov, NCT04361994, https://clinicaltrials.gov/study/NCT04361994
Results
Of the 2453 TTS patients discharged alive, 1683 (68%) received RASi therapy. Patients with RASi were older (age 71 ± 11 vs 69 ± 13 years, P = .01), with higher prevalence of hypertension (74% vs 53%, P < .01) and diabetes (19% v s15%, P = .01), higher admission left ventricular ejection fraction (LVEF) (41 ± 11% vs 39 ± 12%, P < .01) and lower rates of in-hospital complications (18.9% vs 29.6%, P < .01). At multivariable analysis, RASi therapy at discharge was independently associated with lower mortality (HR 0.63, 95% CI 0.45-0.87, P < .01). Survival analysis showed that at long term, patients treated with RASi had lower mortality rates in the overall cohort (log-rank P = .001). However, this benefit was not found among patients treated with RASi in the matched cohort (log-rank P = .168). Potential survival benefit of RASi were present, both in the overall and matched cohort, in 2 subgroups: patients with admission LVEF ≤ 40% (HR 0.54 95% CI 0.38-0.78, P = .001; HR 0.59, 95% CI 0.37-0.95, P = .030) and diabetes (HR 0.41, 95% CI 0.23-0.73, P = .002; HR 0.41, 95% CI 0.21-0.82, P = .011).
Conclusions
Long-term therapy with RASi after a TTS episode was not associated with lower mortality rates at propensity score analysis. However, potential survival benefit can be found among patients with admission LVEF ≤ 40% or diabetes.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American heart journal
医学-心血管系统
CiteScore
8.20
自引率
2.10%
发文量
214
审稿时长
38 days
期刊介绍:
The American Heart Journal will consider for publication suitable articles on topics pertaining to the broad discipline of cardiovascular disease. Our goal is to provide the reader primary investigation, scholarly review, and opinion concerning the practice of cardiovascular medicine. We especially encourage submission of 3 types of reports that are not frequently seen in cardiovascular journals: negative clinical studies, reports on study designs, and studies involving the organization of medical care. The Journal does not accept individual case reports or original articles involving bench laboratory or animal research.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


