在非酒精性脂肪性肝炎中,HIF-2α 驱动肝 Kupffer 细胞死亡和促炎性招募的巨噬细胞活化
IF 15.8
1区 医学
Q1 CELL BIOLOGY
引用次数: 0
摘要
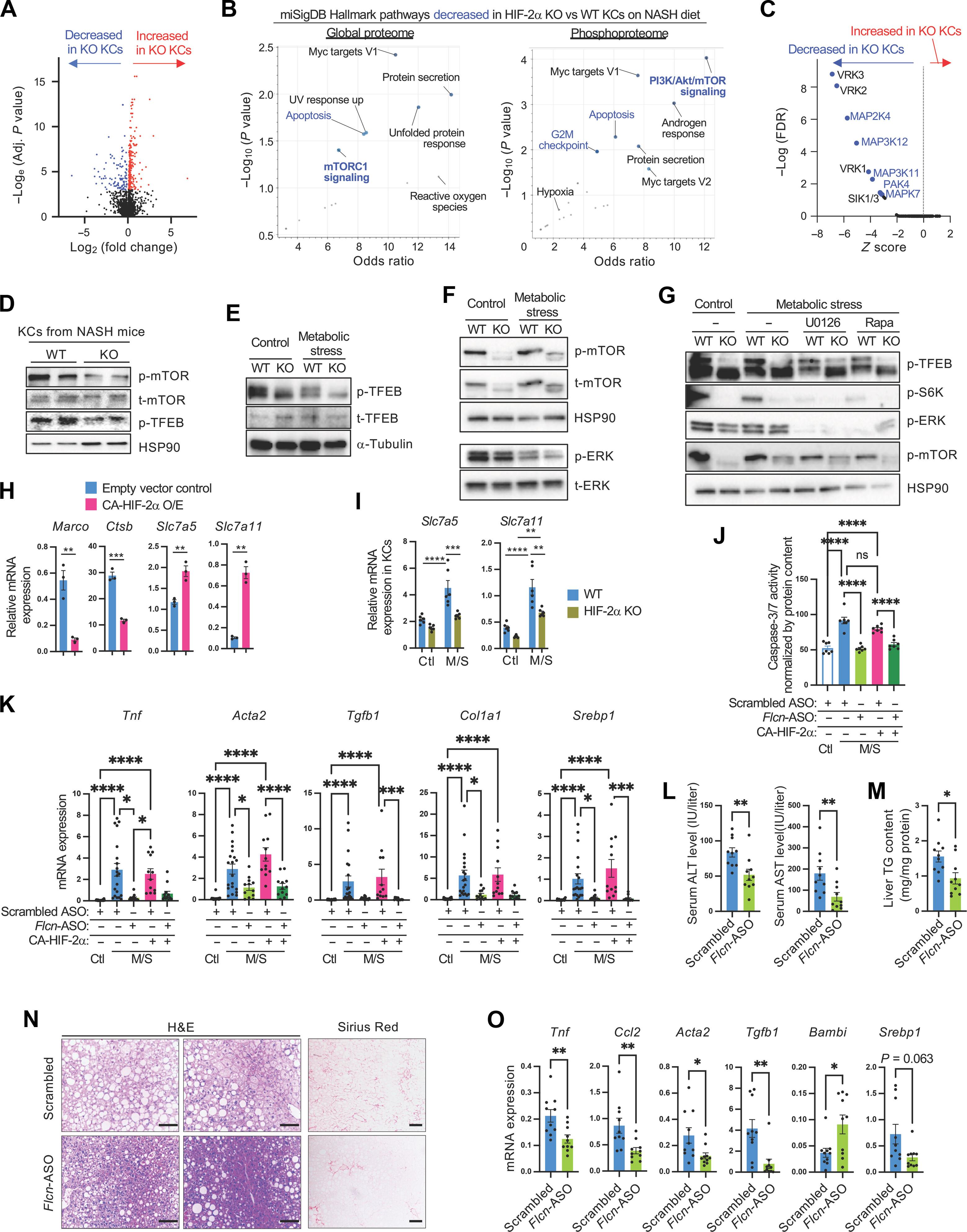
促炎性肝巨噬细胞活化在非酒精性脂肪性肝炎(NASH)的发病过程中起着关键作用。这涉及胚胎肝 Kupffer 细胞(KC)死亡的增加,促进了骨髓来源的高表达促炎基因的招募肝巨噬细胞(RHM)对 KC 的替代。此外,在 NASH 中,KCs 的噬细胞/吞噬细胞活性减弱,从而加剧了肝脏炎症。然而,KCs 发生这些变化的分子机制尚不清楚。在这里,我们发现低氧诱导因子2α(HIF-2α)通过增强溶酶体应激介导了NASH相关的KC生长和排泄减少。在分子水平上,HIF-2α刺激哺乳动物雷帕霉素靶标(mTOR)和细胞外信号调节激酶依赖性抑制转录因子EB(TFEB)磷酸化,导致溶酶体和吞噬基因表达减少。随着 NASH 代谢应激和噬血细胞/吞噬细胞负担的增加,这些变化足以增加溶酶体应激,导致渗出细胞减少和溶酶体细胞死亡。值得注意的是,依赖于 HIF-2α 的 TFEB 调节只发生在 KCs 中,而不是 RHMs 中。相反,在 RHMs 中,HIF-2α 通过增加 ANT2 的表达和线粒体通透性转换,促进线粒体活性氧的产生和促炎激活。因此,髓系特异性或 KC 特异性 HIF-2α 消耗或使用反义寡核苷酸抑制依赖于 mTOR 的 TFEB 抑制可防止小鼠发生 NASH。此外,HIF-2α特异性抑制剂还能减少在类似NASH条件下培养的人肝球细胞中炎症和纤维化基因的表达。总之,我们的研究结果表明,HIF-2α对巨噬细胞亚型的特异性作用共同促成了肝脏巨噬细胞的促炎激活,从而导致了NASH的发生。本文章由计算机程序翻译,如有差异,请以英文原文为准。
HIF-2α drives hepatic Kupffer cell death and proinflammatory recruited macrophage activation in nonalcoholic steatohepatitis
Proinflammatory hepatic macrophage activation plays a key role in the development of nonalcoholic steatohepatitis (NASH). This involves increased embryonic hepatic Kupffer cell (KC) death, facilitating the replacement of KCs with bone marrow–derived recruited hepatic macrophages (RHMs) that highly express proinflammatory genes. Moreover, phago/efferocytic activity of KCs is diminished in NASH, enhancing liver inflammation. However, the molecular mechanisms underlying these changes in KCs are not known. Here, we show that hypoxia-inducible factor 2α (HIF-2α) mediates NASH-associated decreased KC growth and efferocytosis by enhancing lysosomal stress. At the molecular level, HIF-2α stimulated mammalian target of rapamycin (mTOR)– and extracellular signal–regulated kinase-dependent inhibitory transcription factor EB (TFEB) phosphorylation, leading to decreased lysosomal and phagocytic gene expression. With increased metabolic stress and phago/efferocytic burden in NASH, these changes were sufficient to increase lysosomal stress, causing decreased efferocytosis and lysosomal cell death. Of interest, HIF-2α–dependent TFEB regulation only occurred in KCs but not RHMs. Instead, in RHMs, HIF-2α promoted mitochondrial reactive oxygen species production and proinflammatory activation by increasing ANT2 expression and mitochondrial permeability transition. Consequently, myeloid lineage–specific or KC-specific HIF-2α depletion or the inhibition of mTOR-dependent TFEB inhibition using antisense oligonucleotide treatment protected against the development of NASH in mice. Moreover, treatment with an HIF-2α–specific inhibitor reduced inflammatory and fibrogenic gene expression in human liver spheroids cultured under a NASH-like condition. Together, our results suggest that macrophage subtype–specific effects of HIF-2α collectively contribute to the proinflammatory activation of liver macrophages, leading to the development of NASH.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
Science Translational Medicine
CELL BIOLOGY-MEDICINE, RESEARCH & EXPERIMENTAL
CiteScore
26.70
自引率
1.20%
发文量
309
审稿时长
1.7 months
期刊介绍:
Science Translational Medicine is an online journal that focuses on publishing research at the intersection of science, engineering, and medicine. The goal of the journal is to promote human health by providing a platform for researchers from various disciplines to communicate their latest advancements in biomedical, translational, and clinical research.
The journal aims to address the slow translation of scientific knowledge into effective treatments and health measures. It publishes articles that fill the knowledge gaps between preclinical research and medical applications, with a focus on accelerating the translation of knowledge into new ways of preventing, diagnosing, and treating human diseases.
The scope of Science Translational Medicine includes various areas such as cardiovascular disease, immunology/vaccines, metabolism/diabetes/obesity, neuroscience/neurology/psychiatry, cancer, infectious diseases, policy, behavior, bioengineering, chemical genomics/drug discovery, imaging, applied physical sciences, medical nanotechnology, drug delivery, biomarkers, gene therapy/regenerative medicine, toxicology and pharmacokinetics, data mining, cell culture, animal and human studies, medical informatics, and other interdisciplinary approaches to medicine.
The target audience of the journal includes researchers and management in academia, government, and the biotechnology and pharmaceutical industries. It is also relevant to physician scientists, regulators, policy makers, investors, business developers, and funding agencies.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


