用于检测颅内高压的深度学习方法的衍生、外部和临床验证
IF 12.4
1区 医学
Q1 HEALTH CARE SCIENCES & SERVICES
引用次数: 0
摘要
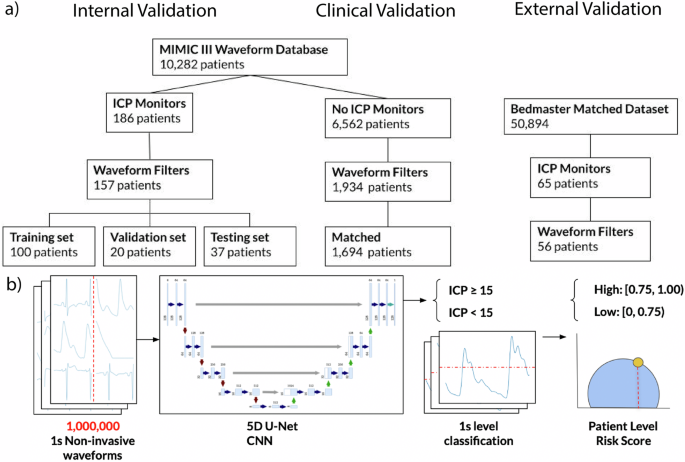
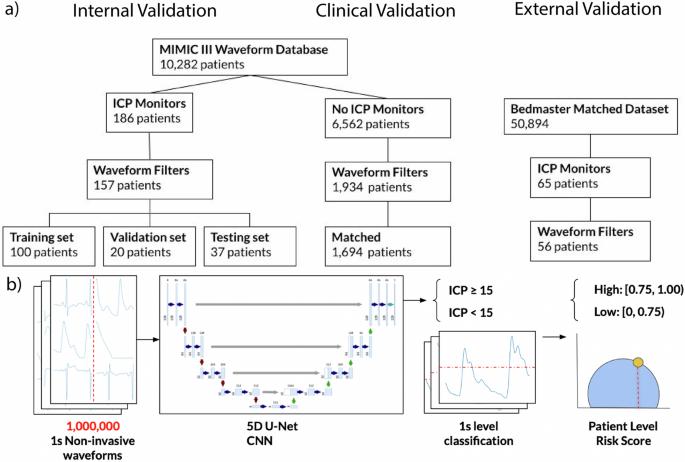
颅内压(ICP)升高≥15 mmHg 与不良的神经系统预后有关,但需要进行有创颅内监测。利用波士顿公开的 MIMIC-III 波形数据库(2000-2013 年),我们为成年患者开发了一种人工智能衍生的 ICP 升高生物标志物(aICP)。我们利用纽约市西奈山医院(2020-2022 年)的独立数据集对 aICP 进行了外部验证。外部验证数据集的 AUROC、准确性、灵敏度和特异性分别为 0.80(95% CI,0.80-0.80)、73.8%(95% CI,72.0-75.6%)、73.5%(95% CI,72.5-74.5%)和 73.0%(95% CI,72.0-74.0%)。我们还进行了一项探索性分析,结果显示 aICP 预测与临床表型有关。10个百分点的增量与脑恶性肿瘤(OR = 1.68; 95% CI, 1.09-2.60)、脑内出血(OR = 1.18; 95% CI, 1.07-1.32)和开颅手术(OR = 1.43; 95% CI, 1.12-1.84;所有P均为0.05)相关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Derivation, external and clinical validation of a deep learning approach for detecting intracranial hypertension
Increased intracranial pressure (ICP) ≥15 mmHg is associated with adverse neurological outcomes, but needs invasive intracranial monitoring. Using the publicly available MIMIC-III Waveform Database (2000–2013) from Boston, we developed an artificial intelligence-derived biomarker for elevated ICP (aICP) for adult patients. aICP uses routinely collected extracranial waveform data as input, reducing the need for invasive monitoring. We externally validated aICP with an independent dataset from the Mount Sinai Hospital (2020–2022) in New York City. The AUROC, accuracy, sensitivity, and specificity on the external validation dataset were 0.80 (95% CI, 0.80–0.80), 73.8% (95% CI, 72.0–75.6%), 73.5% (95% CI 72.5–74.5%), and 73.0% (95% CI, 72.0–74.0%), respectively. We also present an exploratory analysis showing aICP predictions are associated with clinical phenotypes. A ten-percentile increment was associated with brain malignancy (OR = 1.68; 95% CI, 1.09-2.60), intracerebral hemorrhage (OR = 1.18; 95% CI, 1.07–1.32), and craniotomy (OR = 1.43; 95% CI, 1.12–1.84; P < 0.05 for all).
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

NPJ Digital Medicine
Multiple-
CiteScore
25.10
自引率
3.30%
发文量
170
审稿时长
15 weeks
期刊介绍:
npj Digital Medicine is an online open-access journal that focuses on publishing peer-reviewed research in the field of digital medicine. The journal covers various aspects of digital medicine, including the application and implementation of digital and mobile technologies in clinical settings, virtual healthcare, and the use of artificial intelligence and informatics.
The primary goal of the journal is to support innovation and the advancement of healthcare through the integration of new digital and mobile technologies. When determining if a manuscript is suitable for publication, the journal considers four important criteria: novelty, clinical relevance, scientific rigor, and digital innovation.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


