妊娠中期宫颈长度正常的妇女在妊娠早期三个月宫颈过短对早产的预测价值。
IF 3.1
2区 医学
Q1 OBSTETRICS & GYNECOLOGY
American Journal of Obstetrics & Gynecology Mfm
Pub Date : 2024-08-30
DOI:10.1016/j.ajogmf.2024.101476
引用次数: 0
摘要
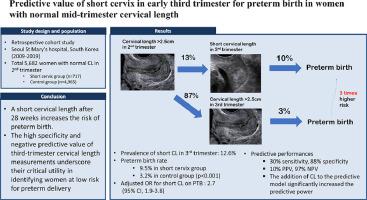
背景妊娠中期宫颈长度过短是早产的有力预测指标。然而,妊娠三个月宫颈长度对预测早产的临床意义尚未确定:研究设计: :这项回顾性队列研究包括在妊娠后三个月(16+0 周至 27+6 周)和妊娠早期三个月(28+0 周至 33+6 周)至少测量过一次宫颈长度的妇女。第二孕期宫颈长度短的妇女、多胎妊娠妇女、接受过宫颈环扎手术的妇女以及先天性早产的妇女被排除在外。研究对象根据怀孕三个月时的宫颈长度分为两组:短宫颈组(≤ 25 毫米)和对照组(> 25 毫米)。两组的早产率(< 37 周)进行了比较。评估了怀孕三个月时宫颈长度对早产的预测性:宫颈长度短于 28+0 至 33+6 周的妇女占总研究人数(5682 人)的 12.6%(717 人)。短宫颈组的早产率为 9.5%,明显高于对照组的 3.2%(P < 0.001)。宫颈长度过短与早产的调整后几率比为 2.73(95% CI:1.96-3.79)。在预测早产方面,第三孕期宫颈短的敏感性为 30.1%,特异性为 88.1%,阳性预测值为 9.5%,阴性预测值为 96.8%。在预测模型中加入第三孕期宫颈长度后,曲线下面积从 0.64 (95% CI: 0.60-0.68) 显著增加到 0.67 (95% CI: 0.63-0.71) (p = 0.002),显示预测性能有所提高:结论:在孕中期宫颈长度正常的妇女中,约有 13% 在 28 周后宫颈长度变短,这增加了早产的风险。第三孕期宫颈长度测量的高特异性和阴性预测值强调了其在识别早产低风险妇女方面的重要作用。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Predictive value of short cervix in early third trimester for preterm birth in women with normal mid-trimester cervical length
Background
Short cervical length in the mid-trimester is a powerful predictor of preterm birth (PTB). However, clinical significance of cervical length in the third trimester for predicting PTB has not been established yet.
Objective
To examine the predictive role of a shortened cervix in the third trimester for PTB in women who had a normal cervical length in the second trimester
Study design
This retrospective cohort study included women who underwent cervical length measured at least once in both the second trimester (16+0 weeks to 27+6weeks) and the early third trimester (28+0 weeks to 33+6 weeks). Women with short cervical length in the second trimester, those with multiple pregnancies, those who underwent cerclage operation, and those who had iatrogenic PTB were excluded. The study population was divided into two groups based on cervical length in the third trimester: a short cervix (≤25 mm) group and a control group (>25 mm). Rates of PTB (<37 weeks) were compared between two groups. Predictive performances of cervical length in the third trimester for PTB were assessed.
Results
Women with a short cervical length at 28+0 to 33+6 weeks accounted for 12.6% (n=717) of the total study population (n=5682). PTB rate was 9.5% in the short cervix group, which was significantly higher than that (3.2%) in the control group (P<.001). The adjusted odds ratio for short cervical length on PTB was 2.73 (95% CI: 1.96–3.79). A short cervix in the third trimester had a sensitivity of 30.1%, a specificity of 88.1%, a positive predictive value of 9.5%, and a negative predictive value (NPV) of 96.8% in predicting PTB. The addition of third-trimester cervical length to the predictive model significantly increased the area under the curve from 0.64 (95% CI: 0.60–0.68) to 0.67 (95% CI: 0.63–0.71) (P=.002), demonstrating improved predictive performance.
Conclusion
Approximately 13% of women with normal cervical length in the mid-trimester had a short cervical length after 28 weeks, which increased the risk of PTB. The high specificity and NPV of third-trimester cervical length measurements underscore their critical utility in identifying women at low risk for preterm delivery.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

American Journal of Obstetrics & Gynecology Mfm
Medicine-Medicine (all)
CiteScore
7.40
自引率
3.20%
发文量
254
审稿时长
40 days
期刊介绍:
The American Journal of Obstetrics and Gynecology (AJOG) is a highly esteemed publication with two companion titles. One of these is the American Journal of Obstetrics and Gynecology Maternal-Fetal Medicine (AJOG MFM), which is dedicated to the latest research in the field of maternal-fetal medicine, specifically concerning high-risk pregnancies. The journal encompasses a wide range of topics, including:
Maternal Complications: It addresses significant studies that have the potential to change clinical practice regarding complications faced by pregnant women.
Fetal Complications: The journal covers prenatal diagnosis, ultrasound, and genetic issues related to the fetus, providing insights into the management and care of fetal health.
Prenatal Care: It discusses the best practices in prenatal care to ensure the health and well-being of both the mother and the unborn child.
Intrapartum Care: It provides guidance on the care provided during the childbirth process, which is critical for the safety of both mother and baby.
Postpartum Issues: The journal also tackles issues that arise after childbirth, focusing on the postpartum period and its implications for maternal health. AJOG MFM serves as a reliable forum for peer-reviewed research, with a preference for randomized trials and meta-analyses. The goal is to equip researchers and clinicians with the most current information and evidence-based strategies to effectively manage high-risk pregnancies and to provide the best possible care for mothers and their unborn children.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


