成人急性髓性白血病异基因造血细胞移植后形态学缓解与血液学恢复之间的关系。
IF 4.5
2区 医学
Q1 HEMATOLOGY
引用次数: 0
摘要
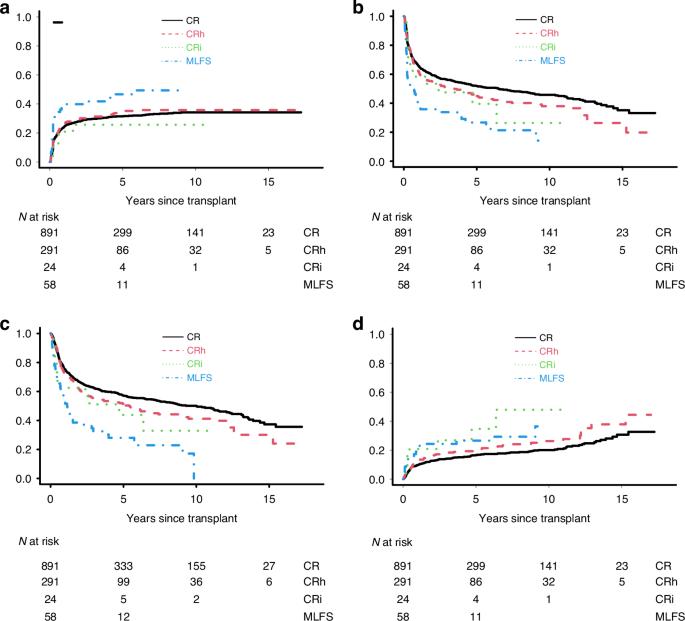
成人急性髓细胞性白血病患者接受异体移植后的预后差别很大。虽然许多协变量与复发、非复发死亡率(NRM)和/或生存期缩短有关,但移植前血细胞计数恢复不完全的影响仍不清楚。为了解决这一不确定性,我们研究了 2006 年至 2023 年期间在一家机构接受异体移植的所有急性髓细胞性白血病或 MDS/AML 成人患者,这些患者在第一次或第二次缓解期接受了异体移植。在 1264 名患者中,891 人(70%)符合 CR 标准,而 291 人(23%)、24 人(2%)和 58 人(5%)分别被归类为 CRh、CRi 和无形态白血病状态(MLFS)。CR、CRh、CRi和MLFS患者在人口统计学、疾病生物学、移植前可测量残留疾病和移植类型方面存在显著差异。经多变量调整后,CRh 和 CRi 患者的预后与 CR 患者无明显差异。相比之下,MLFS 患者的预后要比 CR 和 CRh 患者差得多,NRM 和复发的风险明显更高,无复发生存期和总生存期明显更短。在几个不同的亚组中也得到了类似的结果。总之,我们的分析提供了经验证据,证明了区分 MLFS 与 CR 和 CRh 患者对于优化风险评估以及可能的个体化治疗决策的重要性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Relationship between morphologic remission with or without hematologic recovery and outcome after allogeneic hematopoietic cell transplantation in adult acute myeloid leukemia
Outcomes of adults with AML after allografting vary widely. While numerous covariates have been associated with relapse, non-relapse mortality (NRM), and/or shorter survival, the impact of incomplete blood count recovery before transplantation has remained unclear. To address this uncertainty, we examined all adults with AML or MDS/AML who received an allograft in first or second remission between 2006 and 2023 at a single institution. Of 1264 patients, 891 (70%) met criteria for CR, whereas 291 (23%), 24 (2%), and 58 (5%) were classified as CRh, CRi, and morphologic leukemia-free state (MLFS), respectively. CR, CRh, CRi, and MLFS patients differed significantly regarding demographics, disease biology, pre-transplant measurable residual disease, and types of transplants. After multivariable adjustment, outcomes for CRh and CRi patients were not significantly different from each other or from those of CR patients. In contrast, outcomes of MLFS patients were substantially worse than those of CR and CRh patients, with significantly higher risk of NRM and relapse, and significantly shorter relapse-free and overall survival. Similar results were obtained in several distinct subsets. Together, our analysis provides empiric evidence for the importance of distinguishing MLFS from CR and CRh patients for optimized risk assessment and, possibly, individualized treatment decision making.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Bone Marrow Transplantation
医学-免疫学
CiteScore
8.40
自引率
8.30%
发文量
337
审稿时长
6 months
期刊介绍:
Bone Marrow Transplantation publishes high quality, peer reviewed original research that addresses all aspects of basic biology and clinical use of haemopoietic stem cell transplantation.
The broad scope of the journal thus encompasses topics such as stem cell biology, e.g., kinetics and cytokine control, transplantation immunology e.g., HLA and matching techniques, translational research, and clinical results of specific transplant protocols. Bone Marrow Transplantation publishes 24 issues a year.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


