Ulgu Arslan, Francijna E. van den Hil, Christine L. Mummery, Valeria Orlova
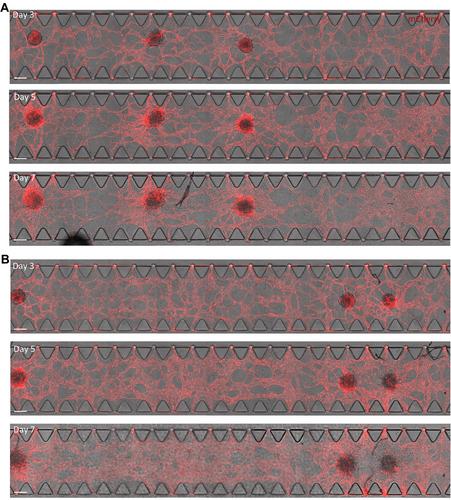
{"title":"hiPSC 衍生的血管化、可灌注心脏芯片微组织的生成与特征描述。","authors":"Ulgu Arslan, Francijna E. van den Hil, Christine L. Mummery, Valeria Orlova","doi":"10.1002/cpz1.1097","DOIUrl":null,"url":null,"abstract":"<p>In the heart <i>in vivo</i>, vasculature forms a semi-permeable endothelial barrier for selective nutrient and (immune) cell delivery to the myocardium and removal of waste products. Crosstalk between the vasculature and the heart cells regulates homeostasis in health and disease. To model heart development and disease <i>in vitro</i> it is important that essential features of this crosstalk are captured. Cardiac organoid and microtissue models often integrate endothelial cells (ECs) to form microvascular networks inside the 3D structure. However, in static culture without perfusion, these networks may fail to show essential functionality. Here, we describe a protocol to generate an <i>in vitro</i> model of human induced pluripotent stem cell (hiPSC)-derived vascularized cardiac microtissues on a microfluidic organ-on-chip platform (VMToC) in which the blood vessels are perfusable. First, prevascularized cardiac microtissues (MT) are formed by combining hiPSC-derived cardiomyocytes, ECs, and cardiac fibroblasts in a pre-defined ratio. Next, these prevascularized MTs are integrated in the chips in a fibrin hydrogel containing additional vascular cells, which self-organize into tubular structures. The MTs become vascularized through anastomosis between the pre-existing microvasculature in the MT and the external vascular network. The VMToCs are then ready for downstream structural and functional assays and basic characterization. Using this protocol, cardiac MTs can be efficiently and robustly vascularized and perfused within 7 days. <i>In vitro</i> vascularized organoid and MT models have the potential to transition current 3D cardiac models to more physiologically relevant organ models that allow the role of the endothelial barrier in drug and inflammatory response to be investigated. © 2024 The Author(s). Current Protocols published by Wiley Periodicals LLC.</p><p><b>Basic Protocol</b>: Generation of VMToC</p><p><b>Support Protocol 1</b>: Functional Characterization of VMToC</p><p><b>Support Protocol 2</b>: Structural Characterization of VMToC</p>","PeriodicalId":93970,"journal":{"name":"Current protocols","volume":"4 7","pages":""},"PeriodicalIF":0.0000,"publicationDate":"2024-07-22","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/cpz1.1097","citationCount":"0","resultStr":"{\"title\":\"Generation and Characterization of hiPSC-Derived Vascularized-, Perfusable Cardiac Microtissues-on-Chip\",\"authors\":\"Ulgu Arslan, Francijna E. van den Hil, Christine L. Mummery, Valeria Orlova\",\"doi\":\"10.1002/cpz1.1097\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>In the heart <i>in vivo</i>, vasculature forms a semi-permeable endothelial barrier for selective nutrient and (immune) cell delivery to the myocardium and removal of waste products. Crosstalk between the vasculature and the heart cells regulates homeostasis in health and disease. To model heart development and disease <i>in vitro</i> it is important that essential features of this crosstalk are captured. Cardiac organoid and microtissue models often integrate endothelial cells (ECs) to form microvascular networks inside the 3D structure. However, in static culture without perfusion, these networks may fail to show essential functionality. Here, we describe a protocol to generate an <i>in vitro</i> model of human induced pluripotent stem cell (hiPSC)-derived vascularized cardiac microtissues on a microfluidic organ-on-chip platform (VMToC) in which the blood vessels are perfusable. First, prevascularized cardiac microtissues (MT) are formed by combining hiPSC-derived cardiomyocytes, ECs, and cardiac fibroblasts in a pre-defined ratio. Next, these prevascularized MTs are integrated in the chips in a fibrin hydrogel containing additional vascular cells, which self-organize into tubular structures. The MTs become vascularized through anastomosis between the pre-existing microvasculature in the MT and the external vascular network. The VMToCs are then ready for downstream structural and functional assays and basic characterization. Using this protocol, cardiac MTs can be efficiently and robustly vascularized and perfused within 7 days. <i>In vitro</i> vascularized organoid and MT models have the potential to transition current 3D cardiac models to more physiologically relevant organ models that allow the role of the endothelial barrier in drug and inflammatory response to be investigated. © 2024 The Author(s). Current Protocols published by Wiley Periodicals LLC.</p><p><b>Basic Protocol</b>: Generation of VMToC</p><p><b>Support Protocol 1</b>: Functional Characterization of VMToC</p><p><b>Support Protocol 2</b>: Structural Characterization of VMToC</p>\",\"PeriodicalId\":93970,\"journal\":{\"name\":\"Current protocols\",\"volume\":\"4 7\",\"pages\":\"\"},\"PeriodicalIF\":0.0000,\"publicationDate\":\"2024-07-22\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://onlinelibrary.wiley.com/doi/epdf/10.1002/cpz1.1097\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"Current protocols\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/cpz1.1097\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"\",\"JCRName\":\"\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"Current protocols","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/cpz1.1097","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"","JCRName":"","Score":null,"Total":0}
引用次数: 0

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


