完全切除的 I-IIIA 期肺癌晚期复发。
IF 4.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-02-01
DOI:10.1016/j.jtcvs.2024.06.026
引用次数: 0
摘要
研究目的对肺腺癌(LUAD)晚期复发(术后2年以上)相关风险因素的研究十分有限。我们研究了与切除的 I-IIIA 期 LUAD 晚期复发相关的发病率、临床病理和基因组特征:我们对完全切除的病理 I-IIIA 期 LUAD 患者(2010-2019 年)进行了回顾性分析。患者均有肺癌病史、新辅助治疗史、粘液性或非侵袭性 LUAD 病史,或随访结果:在纳入的 2349 例患者中,有 537 例在随访期间复发。大多数复发(55% [297/537])发生在早期;45%(240/537)发生在晚期。晚期复发的局部比例高于早期复发(37% vs. 29%; p=0.047)。与未复发患者相比,晚期复发患者的病理特征更具侵袭性(IASLC 2级和3级、淋巴管侵犯、内脏胸膜侵犯),分期也更高。早期和晚期复发患者的病理特征相似,只是早期复发患者中IIIA期疾病更为常见。没有基因组突变与晚期复发有关:结论:LUAD切除术后晚期复发比之前报道的更为常见。术后2年以上未发病且切除时具有侵袭性病理特征的患者复发风险较高,可能会从更积极的随访中获益。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Late recurrence of completely resected stage I to IIIA lung adenocarcinoma
Objective
Research into the risk factors associated with late recurrence (>2 years after surgery) of lung adenocarcinoma is limited. We investigated the incidence of and clinicopathologic and genomic features associated with late recurrence of resected stage I-IIIA lung adenocarcinoma.
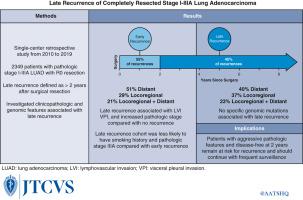
Methods
We performed a retrospective analysis of patients with completely resected pathologic stage I-IIIA lung adenocarcinoma (2010-2019). Patients with a history of lung cancer, neoadjuvant therapy, or mucinous or noninvasive lung adenocarcinoma, or with follow-up of less than 2 years were excluded. Cox and logistic regression modeling were used to compare clinicopathologic variables among patients with no, early (≤2 years), and late recurrence. Comparisons of genomic mutations were corrected for multiple testing.
Results
Of the 2349 patients included, 537 developed a recurrence during follow-up. Most recurrences (55% [297/537]) occurred early; 45% (240/537) occurred late. A larger proportion of late recurrences than early recurrences were locoregional (37% vs 29%; P = .047). Patients with late recurrence had more aggressive pathologic features (International Association for the Study of Lung Cancer grade 2 and 3, lymphovascular invasion, visceral pleural invasion) and higher stage than patients without recurrence. Pathologic features were similar between patients with early and late recurrence, except stage IIIA disease was more common in the early cohort. No genomic mutations were associated with late recurrence.
Conclusions
Late recurrence of lung adenocarcinoma after resection is more common than previously reported. Patients without disease more than 2 years after surgery who had aggressive pathologic features at the time of resection have an elevated risk of recurrence and may benefit from more aggressive follow-up.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


