Tamara Cubiella, Lucía Celada, Jaime San-Juan-Guardado, Raúl Rodríguez-Aguilar, Álvaro Suárez-Priede, María Poch, Francisco Dominguez, Iván Fernández-Vega, Pedro Montero-Pavón, Mario F Fraga, Yoichiro Nakatani, So Takata, Shinichi Yachida, Nuria Valdés, María-Dolores Chiara
下载PDF
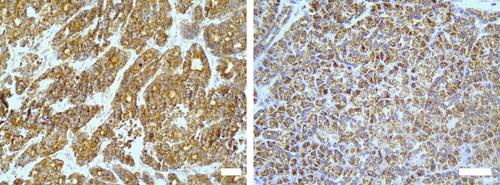
{"title":"PCDHGC3高甲基化作为肠神经内分泌癌的潜在生物标记物","authors":"Tamara Cubiella, Lucía Celada, Jaime San-Juan-Guardado, Raúl Rodríguez-Aguilar, Álvaro Suárez-Priede, María Poch, Francisco Dominguez, Iván Fernández-Vega, Pedro Montero-Pavón, Mario F Fraga, Yoichiro Nakatani, So Takata, Shinichi Yachida, Nuria Valdés, María-Dolores Chiara","doi":"10.1002/path.6291","DOIUrl":null,"url":null,"abstract":"<p>Neuroendocrine neoplasms (NENs) encompass tumors arising from neuroendocrine cells in various organs, including the gastrointestinal tract, pancreas, adrenal gland, and paraganglia. Despite advancements, accurately predicting the aggressiveness of gastroenteropancreatic (GEP) NENs based solely on pathological data remains challenging, thereby limiting optimal clinical management. Our previous research unveiled a crucial link between hypermethylation of the protocadherin <i>PCDHGC3</i> gene and neuroendocrine tumors originating from the paraganglia and adrenal medulla. This epigenetic alteration was associated with increased metastatic potential and succinate dehydrogenase complex (SDH) dysfunction. Expanding upon this discovery, the current study explored <i>PCDHGC3</i> gene methylation within the context of GEP-NENs in a cohort comprising 34 cases. We uncovered promoter hypermethylation of <i>PCDHGC3</i> in 29% of GEP-NENs, with a significantly higher prevalence in gastrointestinal (GI) neuroendocrine carcinomas (NECs) compared with both pancreatic (Pan) NECs and neuroendocrine tumors (NETs) of GI and Pan origin. Importantly, these findings were validated in one of the largest multi-center GEP-NEN cohorts. Mechanistic analysis revealed that <i>PCDHGC3</i> hypermethylation was not associated with <i>SDH</i> mutations or protein loss, indicating an SDH-independent epigenetic mechanism. Clinically, <i>PCDHGC3</i> hypermethylation emerged as a significant prognostic factor, correlating with reduced overall survival rates in both patient cohorts. Significantly, whereas <i>PCDHGC3</i> hypermethylation exhibited a strong correlation with <i>TP53</i> somatic mutations, a hallmark of NEC, its predictive value surpassed that of <i>TP53</i> mutations, with an area under the curve (AUC) of 0.95 (95% CI 0.83–1.0) for discriminating GI-NECs from GI-NETs, highlighting its superior predictive performance. In conclusion, our findings position <i>PCDHGC3</i> methylation status as a promising molecular biomarker for effectively stratifying patients with GI-NENs. This discovery has the potential to advance patient care by enabling more precise risk assessments and tailored treatment strategies. © 2024 The Authors. <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>","PeriodicalId":232,"journal":{"name":"The Journal of Pathology","volume":"263 4-5","pages":"418-428"},"PeriodicalIF":5.6000,"publicationDate":"2024-05-25","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6291","citationCount":"0","resultStr":"{\"title\":\"PCDHGC3 hypermethylation as a potential biomarker of intestinal neuroendocrine carcinomas\",\"authors\":\"Tamara Cubiella, Lucía Celada, Jaime San-Juan-Guardado, Raúl Rodríguez-Aguilar, Álvaro Suárez-Priede, María Poch, Francisco Dominguez, Iván Fernández-Vega, Pedro Montero-Pavón, Mario F Fraga, Yoichiro Nakatani, So Takata, Shinichi Yachida, Nuria Valdés, María-Dolores Chiara\",\"doi\":\"10.1002/path.6291\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>Neuroendocrine neoplasms (NENs) encompass tumors arising from neuroendocrine cells in various organs, including the gastrointestinal tract, pancreas, adrenal gland, and paraganglia. Despite advancements, accurately predicting the aggressiveness of gastroenteropancreatic (GEP) NENs based solely on pathological data remains challenging, thereby limiting optimal clinical management. Our previous research unveiled a crucial link between hypermethylation of the protocadherin <i>PCDHGC3</i> gene and neuroendocrine tumors originating from the paraganglia and adrenal medulla. This epigenetic alteration was associated with increased metastatic potential and succinate dehydrogenase complex (SDH) dysfunction. Expanding upon this discovery, the current study explored <i>PCDHGC3</i> gene methylation within the context of GEP-NENs in a cohort comprising 34 cases. We uncovered promoter hypermethylation of <i>PCDHGC3</i> in 29% of GEP-NENs, with a significantly higher prevalence in gastrointestinal (GI) neuroendocrine carcinomas (NECs) compared with both pancreatic (Pan) NECs and neuroendocrine tumors (NETs) of GI and Pan origin. Importantly, these findings were validated in one of the largest multi-center GEP-NEN cohorts. Mechanistic analysis revealed that <i>PCDHGC3</i> hypermethylation was not associated with <i>SDH</i> mutations or protein loss, indicating an SDH-independent epigenetic mechanism. Clinically, <i>PCDHGC3</i> hypermethylation emerged as a significant prognostic factor, correlating with reduced overall survival rates in both patient cohorts. Significantly, whereas <i>PCDHGC3</i> hypermethylation exhibited a strong correlation with <i>TP53</i> somatic mutations, a hallmark of NEC, its predictive value surpassed that of <i>TP53</i> mutations, with an area under the curve (AUC) of 0.95 (95% CI 0.83–1.0) for discriminating GI-NECs from GI-NETs, highlighting its superior predictive performance. In conclusion, our findings position <i>PCDHGC3</i> methylation status as a promising molecular biomarker for effectively stratifying patients with GI-NENs. This discovery has the potential to advance patient care by enabling more precise risk assessments and tailored treatment strategies. © 2024 The Authors. <i>The Journal of Pathology</i> published by John Wiley & Sons Ltd on behalf of The Pathological Society of Great Britain and Ireland.</p>\",\"PeriodicalId\":232,\"journal\":{\"name\":\"The Journal of Pathology\",\"volume\":\"263 4-5\",\"pages\":\"418-428\"},\"PeriodicalIF\":5.6000,\"publicationDate\":\"2024-05-25\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://onlinelibrary.wiley.com/doi/epdf/10.1002/path.6291\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"The Journal of Pathology\",\"FirstCategoryId\":\"3\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/path.6291\",\"RegionNum\":2,\"RegionCategory\":\"医学\",\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q1\",\"JCRName\":\"ONCOLOGY\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"The Journal of Pathology","FirstCategoryId":"3","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/path.6291","RegionNum":2,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q1","JCRName":"ONCOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


