基于放射组学的机器学习术前预测临床IA期纯固态非小细胞肺癌的生存结果
IF 4.4
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-01-01
DOI:10.1016/j.jtcvs.2024.05.010
引用次数: 0
摘要
目的:临床IA期非小细胞肺癌(NSCLC)在计算机断层扫描(CT)上显示为纯固性,预后较差。本研究旨在利用术前临床和放射学特征开发和验证机器学习模型,以预测临床ⅠA期纯固相非小细胞肺癌的总生存率(OS):方法:对2012年1月至2020年12月期间因NSCLC接受肺切除术的患者进行回顾性研究。方法:对 2012 年 1 月至 2020 年 12 月间接受肺切除术的 NSCLC 患者进行回顾性研究,从 CT 上的瘤内和瘤周区域提取放射学特征。使用随机生存森林(RSF)和 XGBoost 算法开发了机器学习模型,并将 Cox 回归模型设为基准。使用随时间变化的综合曲线下面积(iAUC)评估模型性能,并通过 5 倍交叉验证进行验证:结果:共纳入642例临床IA期纯固NSCLC患者。在3748个放射学特征和34个术前临床特征中,选出了42个特征。两种机器学习模型的表现均优于 Cox 回归模型(iAUC, 0.753 [95% CI: 0.629, 0.829])。XGBoost 模型的表现(iAUC, 0.832 [95% CI: 0.779, 0.880])优于 RSF 模型(iAUC, 0.795 [95% CI: 0.734, 0.856])。XGBoost模型显示了出色的生存分层性能,低风险组(5年OS:100.0%)、中度低风险组(5年OS:88.5%)、中度高风险组(5年OS:75.6%)和高风险组(5年OS:41.7%)的总生存率(OS)差异显著(P < 0.0001):基于放射组学的机器学习模型可以在术前准确预测临床IA期纯固相NSCLC的OS并改善生存分层。本文章由计算机程序翻译,如有差异,请以英文原文为准。
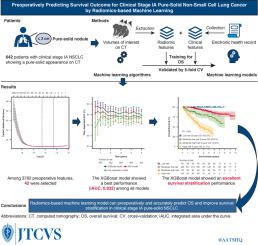
Preoperatively predicting survival outcome for clinical stage IA pure-solid non–small cell lung cancer by radiomics-based machine learning
Objective
Clinical stage IA non–small cell lung cancer (NSCLC) showing a pure-solid appearance on computed tomography is associated with a worse prognosis. This study aimed to develop and validate machine-learning models using preoperative clinical and radiomic features to predict overall survival (OS) in clinical stage IA pure-solid NSCLC.
Methods
Patients who underwent lung resection for NSCLC between January 2012 and December 2020 were reviewed. The radiomic features were extracted from the intratumoral and peritumoral regions on computed tomography. The machine-learning models were developed using random survival forest and eXtreme Gradient Boosting (XGBoost) algorithms, whereas the Cox regression model was set as a benchmark. Model performance was assessed using the integrated time-dependent area under the curve (iAUC) and validated by 5-fold cross-validation.
Results
In total, 642 patients with clinical stage IA pure-solid NSCLC were included. Among 3748 radiomic and 34 preoperative clinical features, 42 features were selected. Both machine-learning models outperformed the Cox regression model (iAUC, 0.753; 95% confidence interval [CI], 0.629-0.829). The XGBoost model showed a better performance (iAUC, 0.832; 95% CI, 0.779-0.880) than the random survival forest model (iAUC, 0.795; 95% CI, 0.734-0.856). The XGBoost model showed an excellent survival stratification performance with a significant OS difference among the low-risk (5-year OS, 100.0%), moderate low-risk (5-year OS, 88.5%), moderate high-risk (5-year OS, 75.6%), and high-risk (5-year OS, 41.7%) groups (P < .0001).
Conclusions
A radiomics-based machine-learning model can preoperatively and accurately predict OS and improve survival stratification in clinical stage IA pure-solid NSCLC.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


