与 I 期肺癌复发相关的高危特征
IF 4.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-02-01
DOI:10.1016/j.jtcvs.2024.05.009
引用次数: 0
摘要
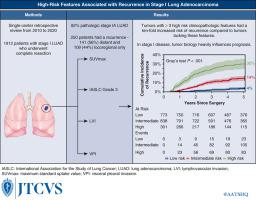
目的:目前对肺腺癌一期(LUAD)的预后特征还缺乏了解。因此,我们研究了与 I 期 LUAD 完全切除术后复发相关的临床病理学特征:我们对 2010 年至 2020 年期间接受 R0 切除术的病理 I 期 LUAD 患者进行了回顾性分析。排除标准包括肺癌病史、诱导或辅助治疗、非侵袭性或粘液性 LUAD 以及术后 90 天内死亡。Fine和Gray竞争风险回归评估了临床病理特征与疾病复发之间的关联:共有1912名患者符合纳入标准。大多数患者(1565 人[82%])为 LUAD IA 期,250 人复发:250人复发:141人(56%)为远处复发,109人(44%)仅为局部复发。5年累计复发率为12%(95%置信区间,11%-14%)。原发肿瘤的最大标准化摄取值较高(危险比[HR]=1.04)、亚肺切除(HR=2.04)、IASLC分级较高(HR=5.32[2级];HR=7.93[3级])、淋巴管侵犯(HR=1.70)、内脏胸膜侵犯(HR=1.54)和肿瘤大小(HR=1.30)与复发的危险性独立相关。具有3-4个高危特征的肿瘤5年后的累积复发率高于不具有这些特征的肿瘤(30%对4%;P结论:I期LUAD患者切除术后的复发仍是一个问题。常见的临床病理特征可用于确定复发风险较高的患者,在评估I期患者的预后时应加以考虑。本文章由计算机程序翻译,如有差异,请以英文原文为准。
High-risk features associated with recurrence in stage I lung adenocarcinoma
Objective
There is a lack of knowledge regarding the use of prognostic features in stage I lung adenocarcinoma (LUAD). Thus, we investigated clinicopathologic features associated with recurrence after complete resection for stage I LUAD.
Methods
We performed a retrospective analysis of patients with pathologic stage I LUAD who underwent R0 resection from 2010 to 2020. Exclusion criteria included history of lung cancer, induction or adjuvant therapy, noninvasive or mucinous LUAD, and death within 90 days of surgery. Fine and Gray competing-risk regression assessed associations between clinicopathologic features and disease recurrence.
Results
In total, 1912 patients met inclusion criteria. Most patients (1565 [82%]) had stage IA LUAD, and 250 developed recurrence: 141 (56%) distant and 109 (44%) locoregional only. The 5-year cumulative incidence of recurrence was 12% (95% CI, 11%-14%). Higher maximum standardized uptake value of the primary tumor (hazard ratio [HR], 1.04), sublobar resection (HR, 2.04), higher International Association for the Study of Lung Cancer grade (HR, 5.32 [grade 2]; HR, 7.93 [grade 3]), lymphovascular invasion (HR, 1.70), visceral pleural invasion (HR, 1.54), and tumor size (HR, 1.30) were independently associated with a hazard of recurrence. Tumors with 3 to 4 high-risk features had a higher cumulative incidence of recurrence at 5 years than tumors without these features (30% vs 4%; P < .001).
Conclusions
Recurrence after resection for stage I LUAD remains an issue for select patients. Commonly reported clinicopathologic features can be used to define patients at high risk of recurrence and should be considered when assessing the prognosis of patients with stage I disease.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


