求助PDF
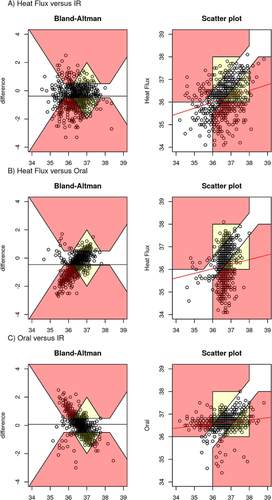
{"title":"剖腹产脊髓麻醉期间三种无创体温监测设备之间的一致性:一项前瞻性观察研究","authors":"DO Vawda, Christopher King, L du Toit, RA Dyer, NJ Masuku, DG Bishop","doi":"10.1007/s10877-024-01154-1","DOIUrl":null,"url":null,"abstract":"<p>Hypothermia during obstetric spinal anaesthesia is a common and important problem, yet temperature monitoring is often not performed due to the lack of a suitable, cost-effective monitor. This study aimed to compare a noninvasive core temperature monitor with two readily available peripheral temperature monitors during obstetric spinal anaesthesia. We undertook a prospective observational study including elective and emergency caesarean deliveries, to determine the agreement between affordable reusable surface temperature monitors (Welch Allyn SureTemp® Plus oral thermometer and the Braun 3-in-1 No Touch infrared thermometer) and the Dräger T-core© (using dual-sensor heat flux technology), in detecting thermoregulatory changes during obstetric spinal anaesthesia. Predetermined clinically relevant limits of agreement (LOA) were set at ± 0.5 °C. We included 166 patients in our analysis. Hypothermia (heat flux temperature < 36 °C) occurred in 67% (95% CI 49 to 78%). There was poor agreement between devices. In the Bland-Altman analysis, LOA for the heat flux monitor vs. oral thermometer were 1.8 °C (CI 1.7 to 2.0 °C; bias 0.5 °C), for heat flux monitor vs. infrared thermometer LOA were 2.3 °C (CI 2.1 to 2.4 °C; bias 0.4 °C) and for infrared vs. oral thermometer, LOA were 2.0 °C (CI 1.9 to 2.2 °C; bias 0.1 °C). Error grid analysis highlighted a large amount of clinical disagreement between methods. While monitoring of core temperature during obstetric spinal anaesthesia is clinically important, agreement between monitors was below clinically acceptable limits. Future research with gold-standard temperature monitors and exploration of causes of sensor divergence is needed.</p>","PeriodicalId":15513,"journal":{"name":"Journal of Clinical Monitoring and Computing","volume":null,"pages":null},"PeriodicalIF":2.0000,"publicationDate":"2024-04-30","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"","citationCount":"0","resultStr":"{\"title\":\"Agreement between three noninvasive temperature monitoring devices during spinal anaesthesia for caesarean delivery: a prospective observational study\",\"authors\":\"DO Vawda, Christopher King, L du Toit, RA Dyer, NJ Masuku, DG Bishop\",\"doi\":\"10.1007/s10877-024-01154-1\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>Hypothermia during obstetric spinal anaesthesia is a common and important problem, yet temperature monitoring is often not performed due to the lack of a suitable, cost-effective monitor. This study aimed to compare a noninvasive core temperature monitor with two readily available peripheral temperature monitors during obstetric spinal anaesthesia. We undertook a prospective observational study including elective and emergency caesarean deliveries, to determine the agreement between affordable reusable surface temperature monitors (Welch Allyn SureTemp® Plus oral thermometer and the Braun 3-in-1 No Touch infrared thermometer) and the Dräger T-core© (using dual-sensor heat flux technology), in detecting thermoregulatory changes during obstetric spinal anaesthesia. Predetermined clinically relevant limits of agreement (LOA) were set at ± 0.5 °C. We included 166 patients in our analysis. Hypothermia (heat flux temperature < 36 °C) occurred in 67% (95% CI 49 to 78%). There was poor agreement between devices. In the Bland-Altman analysis, LOA for the heat flux monitor vs. oral thermometer were 1.8 °C (CI 1.7 to 2.0 °C; bias 0.5 °C), for heat flux monitor vs. infrared thermometer LOA were 2.3 °C (CI 2.1 to 2.4 °C; bias 0.4 °C) and for infrared vs. oral thermometer, LOA were 2.0 °C (CI 1.9 to 2.2 °C; bias 0.1 °C). Error grid analysis highlighted a large amount of clinical disagreement between methods. While monitoring of core temperature during obstetric spinal anaesthesia is clinically important, agreement between monitors was below clinically acceptable limits. Future research with gold-standard temperature monitors and exploration of causes of sensor divergence is needed.</p>\",\"PeriodicalId\":15513,\"journal\":{\"name\":\"Journal of Clinical Monitoring and Computing\",\"volume\":null,\"pages\":null},\"PeriodicalIF\":2.0000,\"publicationDate\":\"2024-04-30\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"Journal of Clinical Monitoring and Computing\",\"FirstCategoryId\":\"3\",\"ListUrlMain\":\"https://doi.org/10.1007/s10877-024-01154-1\",\"RegionNum\":3,\"RegionCategory\":\"医学\",\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q2\",\"JCRName\":\"ANESTHESIOLOGY\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"Journal of Clinical Monitoring and Computing","FirstCategoryId":"3","ListUrlMain":"https://doi.org/10.1007/s10877-024-01154-1","RegionNum":3,"RegionCategory":"医学","ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ANESTHESIOLOGY","Score":null,"Total":0}
引用次数: 0
引用
批量引用

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


