小儿肾移植受者抗体介导的排斥反应:小儿肾脏病研究联合会的报告
IF 1.2
4区 医学
Q3 PEDIATRICS
引用次数: 0
摘要
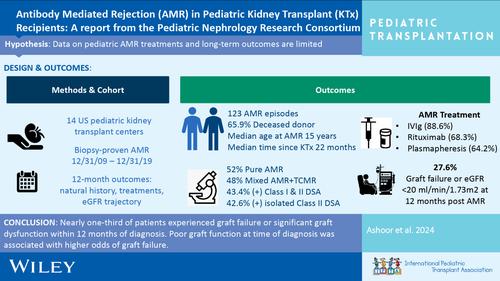
背景抗体介导的排斥反应(AMR)是造成肾脏异体移植损失的主要原因。有关 AMR 治疗结果的大规模儿科特定数据很少。2009年至2019年期间,年龄在1-18岁的肾移植受者在移植时经活检证实患有AMR,并接受了至少12个月的随访。主要结果是移植失败或AMR治疗后12个月的eGFR<20 mL/min/1.73 m2。我们还对AMR治疗选择、组织病理学和DSA分级进行了研究。中位诊断年龄为 15 岁,中位移植时间为 22 个月。确诊 AMR 时,eGFR <30 m/min/1.73 m2 与达到综合结果的风险高出 5.6 倍有关。不同治疗方式的结果无明显差异。在这一庞大的AMR小儿肾移植受者队列中,近三分之一的患者在确诊后12个月内出现移植失败或严重的移植功能障碍。诊断时移植物功能不佳与移植物失败的几率较高有关。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Antibody‐mediated rejection in pediatric kidney transplant recipients: A report from the Pediatric Nephrology Research Consortium
BackgroundAntibody‐mediated rejection (AMR) is a major cause of kidney allograft loss. There is a paucity of large‐scale pediatric‐specific data regarding AMR treatment outcomes.MethodsData were obtained from 14 centers within the Pediatric Nephrology Research Consortium. Kidney transplant recipients aged 1–18 years at transplant with biopsy‐proven AMR between 2009 and 2019 and at least 12 months of follow‐up were included. The primary outcome was graft failure or an eGFR <20 mL/min/1.73 m2 at 12 months following AMR treatment. AMR treatment choice, histopathology, and DSA class were also examined.ResultsWe reviewed 123 AMR episodes. Median age at diagnosis was 15 years at a median 22 months post‐transplant. The primary outcome developed in 27.6%. eGFR <30 m/min/1.73 m2 at AMR diagnosis was associated with a 5.6‐fold higher risk of reaching the composite outcome. There were no significant differences in outcome by treatment modality. Histopathology scores and DSA class at time of AMR diagnosis were not significantly associated with the primary outcome.ConclusionsIn this large cohort of pediatric kidney transplant recipients with AMR, nearly one‐third of patients experienced graft failure or significant graft dysfunction within 12 months of diagnosis. Poor graft function at time of diagnosis was associated with higher odds of graft failure.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Pediatric Transplantation
医学-小儿科
CiteScore
2.90
自引率
15.40%
发文量
216
审稿时长
3-8 weeks
期刊介绍:
The aim of Pediatric Transplantation is to publish original articles of the highest quality on clinical experience and basic research in transplantation of tissues and solid organs in infants, children and adolescents. The journal seeks to disseminate the latest information widely to all individuals involved in kidney, liver, heart, lung, intestine and stem cell (bone-marrow) transplantation. In addition, the journal publishes focused reviews on topics relevant to pediatric transplantation as well as timely editorial comment on controversial issues.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


