接受 CALGB 90401(联盟)治疗的前列腺癌患者发生贝伐珠单抗相关消化道出血的药物遗传学和临床风险因素。
IF 2.9
3区 医学
Q2 GENETICS & HEREDITY
引用次数: 0
摘要
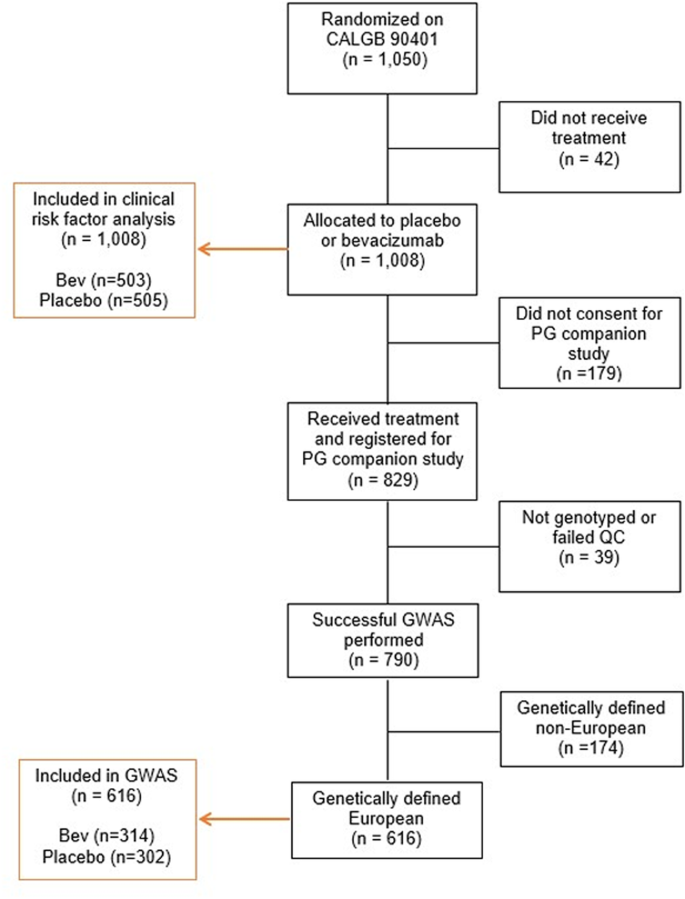
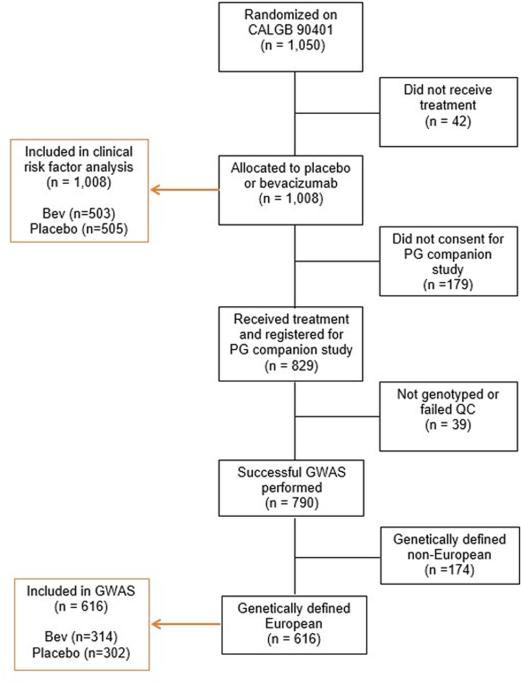
本研究旨在发现与贝伐珠单抗相关的胃肠道出血的临床和药物遗传学因素,研究对象为癌症和白血病 B 组(联盟)90401 例患者。转移性阉割耐药前列腺癌患者接受多西他赛和泼尼松以及贝伐珠单抗治疗。使用 Illumina HumanHap610-Quad 对患者进行基因分型,并使用病因特异性风险评估单核苷酸多态性 (SNP) 与胃肠道出血之间的关联。在1008例患者中,贝伐珠单抗(n = 503)和安慰剂(n = 505)治疗患者中分别有9.5%和3.8%发生2级或2级以上胃肠道出血。贝伐单抗(P -8)超过了 Bonferroni 校正的显著性。贝伐单抗治疗的 AA/AG 和 GG 基因型患者中,2 级或以上胃肠道出血率分别为 33.3% 和 6.2%,而安慰剂组分别为 2.9% 和 1.9%。需要对这些发现进行前瞻性验证和功能分析,以更好地了解基因对治疗相关胃肠道出血的影响。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Pharmacogenetic and clinical risk factors for bevacizumab-related gastrointestinal hemorrhage in prostate cancer patients treated on CALGB 90401 (Alliance)
The objective of this study was to discover clinical and pharmacogenetic factors associated with bevacizumab-related gastrointestinal hemorrhage in Cancer and Leukemia Group B (Alliance) 90401. Patients with metastatic castration-resistant prostate cancer received docetaxel and prednisone ± bevacizumab. Patients were genotyped using Illumina HumanHap610-Quad and assessed using cause-specific risk for association between single nucleotide polymorphisms (SNPs) and gastrointestinal hemorrhage. In 1008 patients, grade 2 or higher gastrointestinal hemorrhage occurred in 9.5% and 3.8% of bevacizumab (n = 503) and placebo (n = 505) treated patients, respectively. Bevacizumab (P < 0.001) and age (P = 0.002) were associated with gastrointestinal hemorrhage. In 616 genetically estimated Europeans (n = 314 bevacizumab and n = 302 placebo treated patients), grade 2 or higher gastrointestinal hemorrhage occurred in 9.6% and 2.0% of patients, respectively. One SNP (rs1478947; HR 6.26; 95% CI 3.19–12.28; P = 9.40 × 10−8) surpassed Bonferroni-corrected significance. Grade 2 or higher gastrointestinal hemorrhage rate was 33.3% and 6.2% in bevacizumab-treated patients with the AA/AG and GG genotypes, versus 2.9% and 1.9% in the placebo arm, respectively. Prospective validation of these findings and functional analyses are needed to better understand the genetic contribution to treatment-related gastrointestinal hemorrhage.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Pharmacogenomics Journal
医学-药学
CiteScore
7.20
自引率
0.00%
发文量
35
审稿时长
6-12 weeks
期刊介绍:
The Pharmacogenomics Journal is a print and electronic journal, which is dedicated to the rapid publication of original research on pharmacogenomics and its clinical applications.
Key areas of coverage include:
Personalized medicine
Effects of genetic variability on drug toxicity and efficacy
Identification and functional characterization of polymorphisms relevant to drug action
Pharmacodynamic and pharmacokinetic variations and drug efficacy
Integration of new developments in the genome project and proteomics into clinical medicine, pharmacology, and therapeutics
Clinical applications of genomic science
Identification of novel genomic targets for drug development
Potential benefits of pharmacogenomics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


