非计划再入院、社区社会经济因素及其对复杂胸主动脉手术后长期生存的影响
IF 4.4
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-01-01
DOI:10.1016/j.jtcvs.2024.01.035
引用次数: 0
摘要
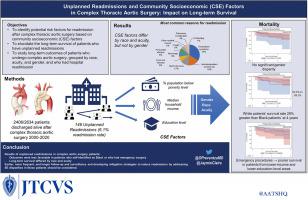
方法 我们按照种族、发病时的敏锐度和性别对指数手术后 60 天内因任何原因再次入院的患者进行了复查。我们还评估了 3 个 CSE 因素:贫困、家庭收入和教育程度。结果在 20 年的研究期间,2406 名患者接受了近端主动脉手术并活着出院,其中我们的团队发现了 146 例(6.1%)计划外再入院患者。与白人患者相比,黑人患者居住的地区贫困现象更普遍(20.8% vs 11.1%,p=.0003),收入更低(42776 美元 vs 65193 美元,p=.0007),拥有高中文凭的居民更少(73.7% vs 90.1%,p <.0001)。与选择性手术的患者相比,紧急或急诊手术的患者居住在收入较低的地区(54,425 美元 vs 64,846 美元,p=.01),拥有高中文凭的居民较少(81.1% vs 89.2%,p=.005)。CSE 因素在性别上没有差异。黑人患者的四年和六年存活率分别为 63.1% 和 63.1%,而白人患者分别为 89.1% 和 83.0%(p=.0009)。结论在再次入院的患者中,黑人患者和接受过急诊手术的患者的CSE因素较差,长期生存率也较低。应考虑更早、更频繁地对这些患者进行随访。针对这些患者发展校外诊所和特定的出院后措施非常重要。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Unplanned readmissions, community socioeconomic factors, and their effects on long-term survival after complex thoracic aortic surgery
Objective
We evaluated community socioeconomic factors in patients who had unplanned readmission after undergoing proximal aortic surgery (ascending aorta, aortic root, or arch).
Methods
Unplanned readmissions for any reason within 60 days of the index procedure were reviewed by race, acuity at presentation, and gender. We also evaluated 3 community socioeconomic factors: poverty, household income, and education. Kaplan-Meier survival curves were used to assess long-term survival differences by group (race, acuity, and gender).
Results
Among 2339 patients who underwent proximal aortic surgery during the 20-year study period and were discharged alive, our team identified 146 (6.2%) unplanned readmissions. Compared with White patients, Black patients lived in areas characterized by more widespread poverty (20.8% vs 11.1%; P = .0003), lower income ($42,776 vs $65,193; P = .0007), and fewer residents with a high school diploma (73.7% vs 90.1%; P < .0001). Compared with patients whose index operation was elective, patients who had urgent or emergency index procedures lived in areas with lower income ($54,425 vs $64,846; P = .01) and fewer residents with a high school diploma (81.1% vs 89.2%; P = .005). Community socioeconomic factors did not differ by gender. Four- and 6-year survival estimates were 63.1% and 63.1% for Black patients versus 89.1% and 83.0% for White patients (P = .0009). No significant differences by acuity or gender were found.
Conclusions
Among readmitted patients, Black patients and patients who had emergency surgery had less favorable community socioeconomic factors and poorer long-term survival. Earlier and more frequent follow-up in these patients should be considered. Developing off-campus clinics and specific postdischarge measures targeting these patients is important.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


