改善急性 A 型主动脉夹层伴灌注不良综合征预后的优化策略
IF 4.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-02-01
DOI:10.1016/j.jtcvs.2024.01.006
引用次数: 0
摘要
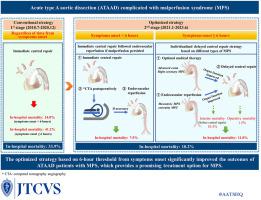
背景急性A型主动脉夹层(ATAAD)合并灌注不良综合征(MPS)的死亡率很高。然而,管理策略仍然存在争议。我们的目标是评估我们机构的MPS策略。方法在724例ATAAD患者中,167例MPS患者采用立即中央修复(一期)或优化策略(二期)进行治疗。在第二阶段,使用的优化策略是基于症状出现后的6小时阈值。对于症状在6小时内出现的MPS,立即进行中央修复,如果持续灌注不良,则进行血管内再灌注。如果症状出现超过6小时,则进行个体化延迟中枢修复。我们比较了第一阶段和第二阶段的结果。结果采用优化策略可显著降低ATAAD患者住院死亡率(第二期4.3% vs第一期12.5%;P & lt;. 01)。在第二阶段,MPS的住院死亡率下降(10.2% vs 33.9%;P & lt;. 01)。此外,症状出现在6小时内和6小时以上的MPS住院死亡率分别从24%下降到7.5%和从41.2%下降到11.8%。MPS二期手术死亡率与无MPS患者相当(4.0% vs 2.4%;P比;. 05)。结论优化后的策略显著提高了MPS的疗效。从症状开始的6小时阈值对于确定中枢修复的时间非常有用。对于6小时内出现MPS症状的患者,立即进行中枢修复是合理的;对于症状发作超过6小时者,应考虑个体化延迟中枢修复。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Optimized strategy to improve the outcomes of acute type A aortic dissection with malperfusion syndrome
Background
The mortality of acute type A aortic dissection (ATAAD) with malperfusion syndrome (MPS) is high. However, the management strategy remains controversial. We aimed to evaluate the strategy for MPS at our institution.
Methods
Among 724 patients with ATAAD, 167 patients with MPS were treated with immediate central repair (first stage) or an optimized strategy (second stage). In the second stage, the optimized strategy used was based on 6-hour threshold from symptom onset. For MPS with symptom onset within 6 hours, immediate central repair was performed, followed by endovascular reperfusion if malperfusion persisted. With symptom onset beyond 6 hours, individualized delayed central repair was performed. We compared outcomes between the first and second stages.
Results
The in-hospital mortality of ATAAD was significantly decreased when the optimized strategy was used (4.3% in the second stage vs 12.5% in the first stage; P < .01). In the second stage, the in-hospital mortality for MPS was decreased (10.2% vs 33.9%; P < .01). Moreover, the in-hospital mortality for MPS with symptom onset within 6 hours and beyond 6 hours decreased from 24% to 7.5% and from 41.2% to 11.8%, respectively. The operative mortality of MPS in the second stage was comparable to that in patients without MPS (4.0% vs 2.4%; P > .05).
Conclusions
The optimized strategy significantly improved the outcomes of MPS. The 6-hour threshold from symptom onset could be very useful in determining the timing of central repair. For patients with MPS symptom onset within 6 hours, immediate central repair is reasonable; for those with symptom onset beyond 6 hours, individualized delayed central repair should be considered.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


