CAR-T 细胞中 SMAD7 的表达提高了治疗实体瘤的持久性和安全性
IF 21.8
1区 医学
Q1 IMMUNOLOGY
引用次数: 0
摘要
尽管嵌合抗原受体T(CAR-T)细胞疗法在血液恶性肿瘤中取得了巨大进展,但其在实体瘤中的应用却受到了限制,这主要是由于T细胞在肿瘤微环境(TME)中耗竭以及细胞因子释放过多导致的全身毒性。作为免疫抑制性 TME 的关键调节因子,TGF-β 通过 NF-κB 通路促进细胞因子的合成。在这里,我们在工程 T 细胞中将 TGF-β 信号抑制因子 SMAD7 与 HER2 靶向 CAR 共表达。这些新型CAR-T细胞显示出很高的细胞溶解效力,并能抵抗TGF-β引发的衰竭,从而在持续暴露于抗原后仍能保持杀瘤能力。此外,SMAD7 还大大减少了抗原刺激 CAR-T 细胞产生的炎性细胞因子。从机理上讲,SMAD7 下调了 TGF-β 受体 I,消减了 CAR-T 细胞中 TGF-β 和 NF-κB 通路之间的相互作用。因此,无论高浓度 TGF-β 导致的恶劣肿瘤微环境如何,这些 CAR-T 细胞都能持续抑制肿瘤生长并促进肿瘤小鼠的存活。SMAD7共表达还增强了CAR-T细胞在患者衍生肿瘤组织细胞中的浸润和持续激活。因此,我们的研究证明了SMAD7共表达作为一种新方法来提高CAR-T细胞治疗实体瘤的疗效和安全性的可行性。本文章由计算机程序翻译,如有差异,请以英文原文为准。
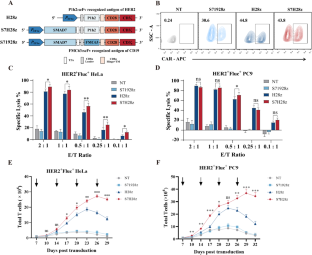
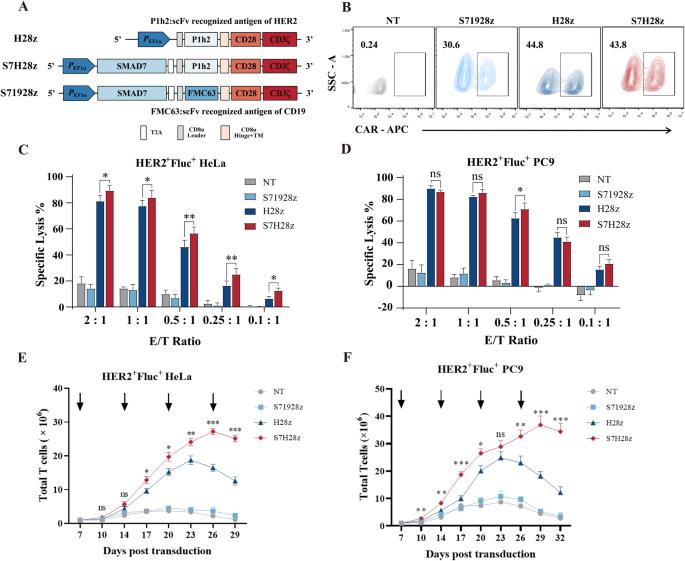
SMAD7 expression in CAR-T cells improves persistence and safety for solid tumors
Despite the tremendous progress of chimeric antigen receptor T (CAR-T) cell therapy in hematological malignancies, their application in solid tumors has been limited largely due to T-cell exhaustion in the tumor microenvironment (TME) and systemic toxicity caused by excessive cytokine release. As a key regulator of the immunosuppressive TME, TGF-β promotes cytokine synthesis via the NF-κB pathway. Here, we coexpressed SMAD7, a suppressor of TGF-β signaling, with a HER2-targeted CAR in engineered T cells. These novel CAR-T cells displayed high cytolytic efficacy and were resistant to TGF-β-triggered exhaustion, which enabled sustained tumoricidal capacity after continuous antigen exposure. Moreover, SMAD7 substantially reduced the production of inflammatory cytokines by antigen-primed CAR-T cells. Mechanistically, SMAD7 downregulated TGF-β receptor I and abrogated the interplay between the TGF-β and NF-κB pathways in CAR-T cells. As a result, these CAR-T cells persistently inhibited tumor growth and promoted the survival of tumor-challenged mice regardless of the hostile tumor microenvironment caused by a high concentration of TGF-β. SMAD7 coexpression also enhanced CAR-T-cell infiltration and persistent activation in patient-derived tumor organoids. Therefore, our study demonstrated the feasibility of SMAD7 coexpression as a novel approach to improve the efficacy and safety of CAR-T-cell therapy for solid tumors.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
31.20
自引率
1.20%
发文量
903
审稿时长
1 months
期刊介绍:
Cellular & Molecular Immunology, a monthly journal from the Chinese Society of Immunology and the University of Science and Technology of China, serves as a comprehensive platform covering both basic immunology research and clinical applications. The journal publishes a variety of article types, including Articles, Review Articles, Mini Reviews, and Short Communications, focusing on diverse aspects of cellular and molecular immunology.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


