基于可解释机器学习的心脏手术患者预后预测模型。
IF 4.9
1区 医学
Q1 CARDIAC & CARDIOVASCULAR SYSTEMS
Journal of Thoracic and Cardiovascular Surgery
Pub Date : 2025-01-01
DOI:10.1016/j.jtcvs.2023.11.034
引用次数: 0
摘要
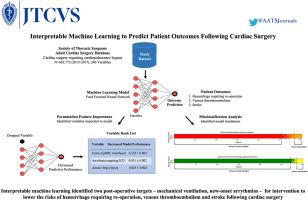
目的:机器学习预测心脏手术后患者预后的临床适用性尚不清楚。我们应用机器学习来预测与心脏手术后高发病率和死亡率相关的患者结果,并确定变量对导出模型性能的重要性。方法:我们将机器学习应用于胸外科学会成人心脏外科数据库,以预测术后出血需要再次手术、静脉血栓栓塞和中风。我们使用排列特征重要性来识别对模型性能重要的变量,并使用错误分类分析来研究模型的局限性。结果:该研究数据集包括2015年至2017年期间接受心脏手术的662,772名受试者和240个变量。再次手术出血、静脉血栓栓塞和脑卒中发生率分别为2.9%、1.2%和2.0%。该模型在预测三种并发症方面表现良好(AUC 0.92-0.97)。术前和术中变量对模型性能不重要。相反,预测所有三种结果的性能主要由几个术后变量驱动,包括已知的并发症危险因素,如机械通气和术后新发心律失常。许多对模型性能重要的术后变量也增加了受试者误分类的风险,表明内部有效性。结论:机器学习模型准确可靠地预测心脏手术后患者的预后。与术前或术中变量相反,术后变量对模型性能很重要。针对这一时期的干预措施,包括减少机械通气的持续时间和早期治疗新发的术后心律失常,可能有助于降低这些并发症的风险。本文章由计算机程序翻译,如有差异,请以英文原文为准。

Interpretable machine learning-based predictive modeling of patient outcomes following cardiac surgery
Background
The clinical applicability of machine learning predictions of patient outcomes following cardiac surgery remains unclear. We applied machine learning to predict patient outcomes associated with high morbidity and mortality after cardiac surgery and identified the importance of variables to the derived model's performance.
Methods
We applied machine learning to the Society of Thoracic Surgeons Adult Cardiac Surgery Database to predict postoperative hemorrhage requiring reoperation, venous thromboembolism (VTE), and stroke. We used permutation feature importance to identify variables important to model performance and a misclassification analysis to study the limitations of the model.
Results
The study dataset included 662,772 subjects who underwent cardiac surgery between 2015 and 2017 and 240 variables. Hemorrhage requiring reoperation, VTE, and stroke occurred in 2.9%, 1.2%, and 2.0% of subjects, respectively. The model performed remarkably well at predicting all 3 complications (area under the receiver operating characteristic curve, 0.92-0.97). Preoperative and intraoperative variables were not important to model performance; instead, performance for the prediction of all 3 outcomes was driven primarily by several postoperative variables, including known risk factors for the complications, such as mechanical ventilation and new onset of postoperative arrhythmias. Many of the postoperative variables important to model performance also increased the risk of subject misclassification, indicating internal validity.
Conclusions
A machine learning model accurately and reliably predicts patient outcomes following cardiac surgery. Postoperative, as opposed to preoperative or intraoperative variables, are important to model performance. Interventions targeting this period, including minimizing the duration of mechanical ventilation and early treatment of new-onset postoperative arrhythmias, may help lower the risk of these complications.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
11.20
自引率
10.00%
发文量
1079
审稿时长
68 days
期刊介绍:
The Journal of Thoracic and Cardiovascular Surgery presents original, peer-reviewed articles on diseases of the heart, great vessels, lungs and thorax with emphasis on surgical interventions. An official publication of The American Association for Thoracic Surgery and The Western Thoracic Surgical Association, the Journal focuses on techniques and developments in acquired cardiac surgery, congenital cardiac repair, thoracic procedures, heart and lung transplantation, mechanical circulatory support and other procedures.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


