孕妇中的COVID-19:关于妊娠丢失风险和流行率的系统回顾和荟萃分析
摘要
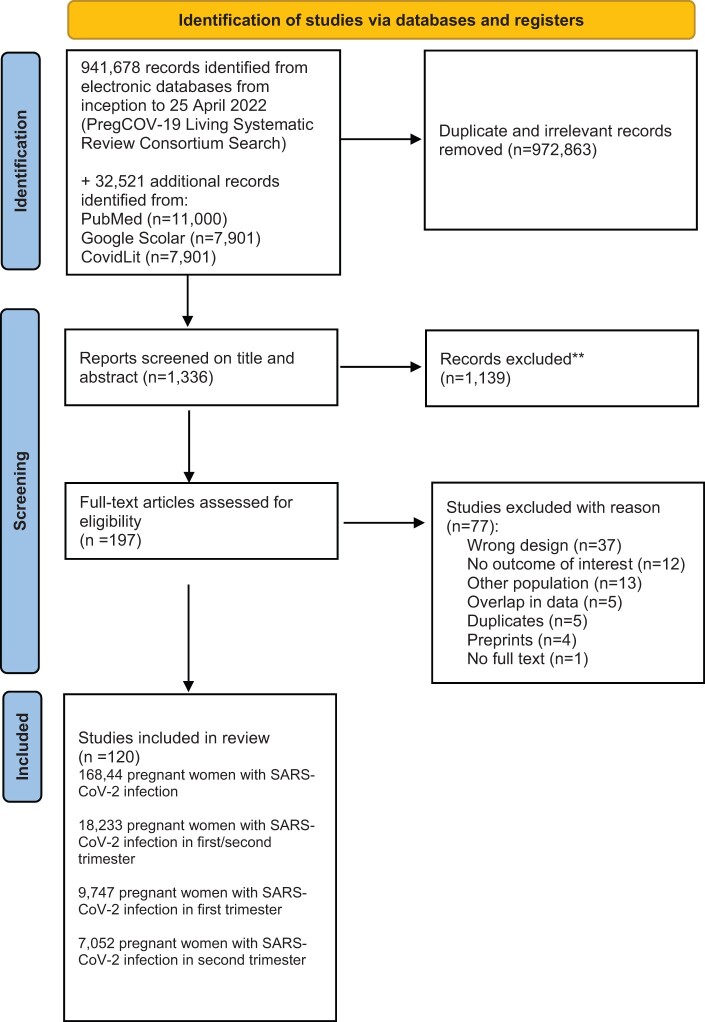
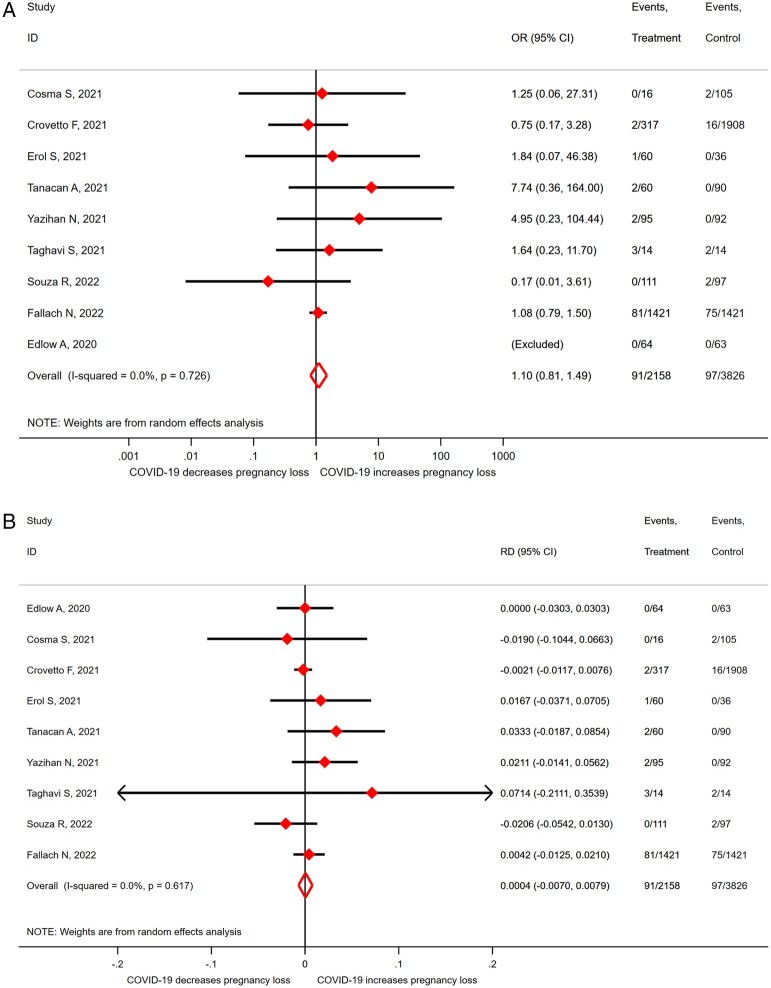
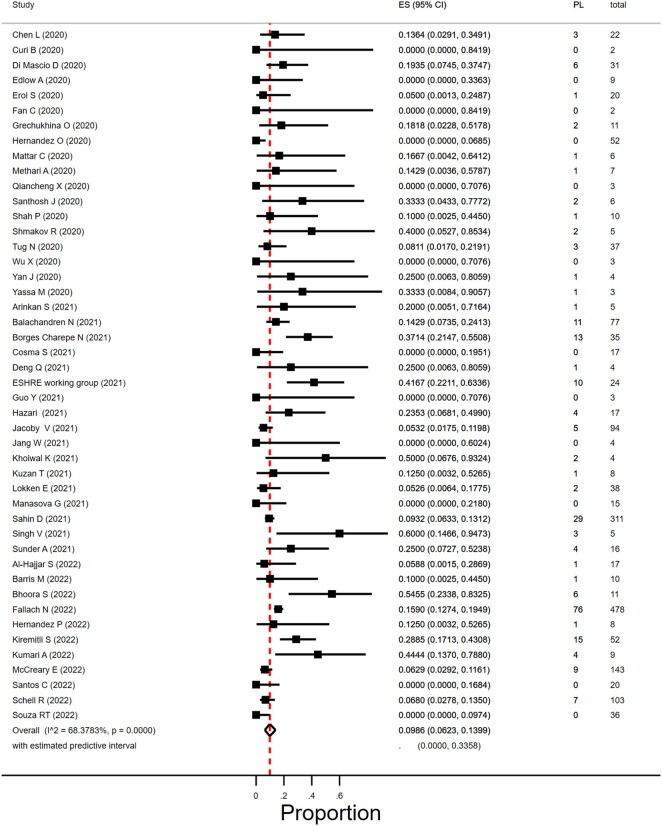
背景:感染了严重急性呼吸综合征冠状病毒2 (SARS-CoV-2)的孕妇更容易出现早产,其新生儿更容易死产或住进新生儿病房。世界卫生组织于2023年5月宣布2019冠状病毒病(COVID-19)大流行结束,这是全球卫生紧急情况。然而,孕妇仍然会感染SARS-CoV-2,并且关于妊娠早期感染SARS-CoV-2对妊娠结局的影响的信息有限。目的和理由:我们进行了本系统综述,以确定感染SARS-Cov-2的妇女早期妊娠流产的发生率,并将其与未感染SARS-Cov-2的孕妇的风险进行比较。检索方法:我们的系统综述基于前瞻性注册方案。在PubMed、Google Scholar和LitCovid中对PregCov19联合体的搜索进行了额外的电子搜索,专门针对截至2023年3月10日感染SARS-CoV-2的孕妇的妊娠损失进行了搜索。我们纳入了SARS-CoV-2感染孕妇的回顾性和前瞻性研究,前提是这些研究包含妊娠早期和/或中期妊娠损失的信息。主要结局是流产,定义为妊娠20周前的流产,然而,报告妊娠22或24周流产的研究也包括在内。此外,我们还报道了一些研究,这些研究将妊娠丢失定义为发生在妊娠的第一个和/或第二个三个月,而没有指定胎龄,并且只有当研究将死产和/或胎儿丢失与流产分开时,才会将妊娠丢失定义为第二个三个月流产。数据分为妊娠早期和中期。次要结局是异位妊娠(任何子宫外妊娠)和终止妊娠。至少有三名研究人员独立提取数据并评估研究质量。我们以相应的95% CI计算优势比(OR)和风险差异(RDs),并使用随机效应荟萃分析汇总数据。为了估计风险患病率,我们对比例进行了荟萃分析。异质性采用I2评估。结果:我们纳入了120项研究,共包括164844名感染SARS-CoV-2的孕妇;其中18233名妇女处于妊娠早期或中期。证据水平被认为是低到中等确定性,主要是由于选择偏差。我们没有发现SARS-CoV-2感染与流产之间存在关联的证据(OR 1.10, 95% CI 0.81-1.48;I2 = 0.0%;RD为0.0012,95% CI为-0.0103 ~ 0.0127;I2 = 0%;9项研究,4439名女性)。流产发生率为9.9% (95% CI 6.2-14.0%;I2 = 68%;46项研究,1797名妇女)在妊娠早期感染SARS - CoV-2的妇女和1.2% (95% CI 0.3-2.4%;i2 = 34%;33个研究;3159名妇女)在妊娠中期。SARS-CoV-2感染妇女宫外孕的比例为1.4% (95% CI 0.02-4.2%;i2 = 66%;14项研究,950名女性)。终止妊娠发生率为0.6% (95% CI 0.01-1.6%;i2 = 79%;39岁的研究;1166名女性)。更广泛的影响:我们的研究发现,没有迹象表明在妊娠早期或中期感染SARS-CoV-2会增加流产的风险。为了提供更好的风险估计,需要设计良好的研究,包括怀孕和妊娠早期感染SARS-CoV-2和未感染SARS-CoV-2的孕妇,并考虑SARS-CoV-2感染的临床表现和严重程度与妊娠丢失的关系,以及潜在的混杂因素,如既往妊娠丢失。在临床实践中,仍应建议孕妇采取预防措施,避免暴露于SARS-CoV-2的风险,并接种SARS-CoV-2疫苗。
Background: Pregnant women infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are more likely to experience preterm birth and their neonates are more likely to be stillborn or admitted to a neonatal unit. The World Health Organization declared in May 2023 an end to the coronavirus disease 2019 (COVID-19) pandemic as a global health emergency. However, pregnant women are still becoming infected with SARS-CoV-2 and there is limited information available regarding the effect of SARS-CoV-2 infection in early pregnancy on pregnancy outcomes.
Objective and rationale: We conducted this systematic review to determine the prevalence of early pregnancy loss in women with SARS-Cov-2 infection and compare the risk to pregnant women without SARS-CoV-2 infection.
Search methods: Our systematic review is based on a prospectively registered protocol. The search of PregCov19 consortium was supplemented with an extra electronic search specifically on pregnancy loss in pregnant women infected with SARS-CoV-2 up to 10 March 2023 in PubMed, Google Scholar, and LitCovid. We included retrospective and prospective studies of pregnant women with SARS-CoV-2 infection, provided that they contained information on pregnancy losses in the first and/or second trimester. Primary outcome was miscarriage defined as a pregnancy loss before 20 weeks of gestation, however, studies that reported loss up to 22 or 24 weeks were also included. Additionally, we report on studies that defined the pregnancy loss to occur at the first and/or second trimester of pregnancy without specifying gestational age, and for second trimester miscarriage only when the study presented stillbirths and/or foetal losses separately from miscarriages. Data were stratified into first and second trimester. Secondary outcomes were ectopic pregnancy (any extra-uterine pregnancy), and termination of pregnancy. At least three researchers independently extracted the data and assessed study quality. We calculated odds ratios (OR) and risk differences (RDs) with corresponding 95% CI and pooled the data using random effects meta-analysis. To estimate risk prevalence, we performed meta-analysis on proportions. Heterogeneity was assessed by I2.
Outcomes: We included 120 studies comprising a total of 168 444 pregnant women with SARS-CoV-2 infection; of which 18 233 women were in their first or second trimester of pregnancy. Evidence level was considered to be of low to moderate certainty, mostly owing to selection bias. We did not find evidence of an association between SARS-CoV-2 infection and miscarriage (OR 1.10, 95% CI 0.81-1.48; I2 = 0.0%; RD 0.0012, 95% CI -0.0103 to 0.0127; I2 = 0%; 9 studies, 4439 women). Miscarriage occurred in 9.9% (95% CI 6.2-14.0%; I2 = 68%; 46 studies, 1797 women) of the women with SARS CoV-2 infection in their first trimester and in 1.2% (95% CI 0.3-2.4%; I2 = 34%; 33 studies; 3159 women) in the second trimester. The proportion of ectopic pregnancies in women with SARS-CoV-2 infection was 1.4% (95% CI 0.02-4.2%; I2 = 66%; 14 studies, 950 women). Termination of pregnancy occurred in 0.6% of the women (95% CI 0.01-1.6%; I2 = 79%; 39 studies; 1166 women).
Wider implications: Our study found no indication that SARS-CoV-2 infection in the first or second trimester increases the risk of miscarriages. To provide better risk estimates, well-designed studies are needed that include pregnant women with and without SARS-CoV-2 infection at conception and early pregnancy and consider the association of clinical manifestation and severity of SARS-CoV-2 infection with pregnancy loss, as well as potential confounding factors such as previous pregnancy loss. For clinical practice, pregnant women should still be advised to take precautions to avoid risk of SARS-CoV-2 exposure and receive SARS-CoV-2 vaccination.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


