R Clay Bunn, Reuben Adatorwovor, Rebecca R Smith, Philip D Ray, Sarah E Fields, Alexander R Keeble, Christopher S Fry, Sasidhar Uppuganti, Jeffry S Nyman, John L Fowlkes, Evangelia Kalaitzoglou
下载PDF
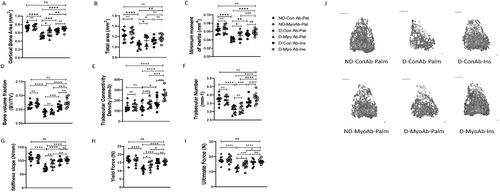
{"title":"肌生长抑制素抗体药物抑制肌生长抑制素改善雄性胰岛素缺乏糖尿病小鼠骨骼肌和骨骼表型","authors":"R Clay Bunn, Reuben Adatorwovor, Rebecca R Smith, Philip D Ray, Sarah E Fields, Alexander R Keeble, Christopher S Fry, Sasidhar Uppuganti, Jeffry S Nyman, John L Fowlkes, Evangelia Kalaitzoglou","doi":"10.1002/jbm4.10833","DOIUrl":null,"url":null,"abstract":"<p>Type 1 diabetes (T1D) is associated with low bone and muscle mass, increased fracture risk, and impaired skeletal muscle function. Myostatin, a myokine that is systemically elevated in humans with T1D, negatively regulates muscle mass and bone formation. We investigated whether pharmacologic myostatin inhibition in a mouse model of insulin-deficient, streptozotocin (STZ)-induced diabetes is protective for bone and skeletal muscle. DBA/2J male mice were injected with low-dose STZ (diabetic) or vehicle (non-diabetic). Subsequently, insulin or palmitate Linbits were implanted and myostatin (REGN647-MyoAb) or control (REGN1945-ConAb) antibody was administered for 8 weeks. Body composition and contractile muscle function were assessed in vivo. Systemic myostatin, P1NP, CTX-I, and glycated hemoglobin (HbA1c) were quantified, and gastrocnemii were weighed and analyzed for muscle fiber composition and gene expression of selected genes. Cortical and trabecular parameters were analyzed (micro-computed tomography evaluations of femur) and cortical bone strength was assessed (three-point bending test of femur diaphysis). In diabetic mice, the combination of insulin/MyoAb treatment resulted in significantly higher lean mass and gastrocnemius weight compared with MyoAb or insulin treatment alone. Similarly, higher raw torque was observed in skeletal muscle of insulin/MyoAb-treated diabetic mice compared with MyoAb or insulin treatment. Additionally, muscle fiber cross-sectional area (CSA) was lower with diabetes and the combination treatment with insulin/MyoAb significantly improved CSA in type II fibers. Insulin, MyoAb, or insulin/MyoAb treatment improved several parameters of trabecular architecture (eg, bone volume fraction [BV/TV], trabecular connectivity density [Conn.D]) and cortical structure (eg, cortical bone area [Ct. Ar.], minimum moment of inertia [Imin]) in diabetic mice. Lastly, cortical bone biomechanical properties (stiffness and yield force) were also improved with insulin or MyoAb treatment. In conclusion, pharmacologic myostatin inhibition is beneficial for muscle mass, muscle function, and bone properties in this mouse model of T1D and its effects are both independent and additive to the positive effects of insulin. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 11","pages":""},"PeriodicalIF":3.4000,"publicationDate":"2023-10-26","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10833","citationCount":"0","resultStr":"{\"title\":\"Pharmacologic Inhibition of Myostatin With a Myostatin Antibody Improves the Skeletal Muscle and Bone Phenotype of Male Insulin-Deficient Diabetic Mice\",\"authors\":\"R Clay Bunn, Reuben Adatorwovor, Rebecca R Smith, Philip D Ray, Sarah E Fields, Alexander R Keeble, Christopher S Fry, Sasidhar Uppuganti, Jeffry S Nyman, John L Fowlkes, Evangelia Kalaitzoglou\",\"doi\":\"10.1002/jbm4.10833\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>Type 1 diabetes (T1D) is associated with low bone and muscle mass, increased fracture risk, and impaired skeletal muscle function. Myostatin, a myokine that is systemically elevated in humans with T1D, negatively regulates muscle mass and bone formation. We investigated whether pharmacologic myostatin inhibition in a mouse model of insulin-deficient, streptozotocin (STZ)-induced diabetes is protective for bone and skeletal muscle. DBA/2J male mice were injected with low-dose STZ (diabetic) or vehicle (non-diabetic). Subsequently, insulin or palmitate Linbits were implanted and myostatin (REGN647-MyoAb) or control (REGN1945-ConAb) antibody was administered for 8 weeks. Body composition and contractile muscle function were assessed in vivo. Systemic myostatin, P1NP, CTX-I, and glycated hemoglobin (HbA1c) were quantified, and gastrocnemii were weighed and analyzed for muscle fiber composition and gene expression of selected genes. Cortical and trabecular parameters were analyzed (micro-computed tomography evaluations of femur) and cortical bone strength was assessed (three-point bending test of femur diaphysis). In diabetic mice, the combination of insulin/MyoAb treatment resulted in significantly higher lean mass and gastrocnemius weight compared with MyoAb or insulin treatment alone. Similarly, higher raw torque was observed in skeletal muscle of insulin/MyoAb-treated diabetic mice compared with MyoAb or insulin treatment. Additionally, muscle fiber cross-sectional area (CSA) was lower with diabetes and the combination treatment with insulin/MyoAb significantly improved CSA in type II fibers. Insulin, MyoAb, or insulin/MyoAb treatment improved several parameters of trabecular architecture (eg, bone volume fraction [BV/TV], trabecular connectivity density [Conn.D]) and cortical structure (eg, cortical bone area [Ct. Ar.], minimum moment of inertia [Imin]) in diabetic mice. Lastly, cortical bone biomechanical properties (stiffness and yield force) were also improved with insulin or MyoAb treatment. In conclusion, pharmacologic myostatin inhibition is beneficial for muscle mass, muscle function, and bone properties in this mouse model of T1D and its effects are both independent and additive to the positive effects of insulin. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>\",\"PeriodicalId\":14611,\"journal\":{\"name\":\"JBMR Plus\",\"volume\":\"7 11\",\"pages\":\"\"},\"PeriodicalIF\":3.4000,\"publicationDate\":\"2023-10-26\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10833\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"JBMR Plus\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10833\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q2\",\"JCRName\":\"ENDOCRINOLOGY & METABOLISM\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10833","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
引用
批量引用

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


