Kyle D Anderson, Christian Beckmann, Saskia Heermant, Frank C Ko, Bryan Dulion, Imad Tarhoni, Jeffrey A Borgia, Amarjit S Virdi, Markus A Wimmer, D Rick Sumner, Ryan D Ross
下载PDF
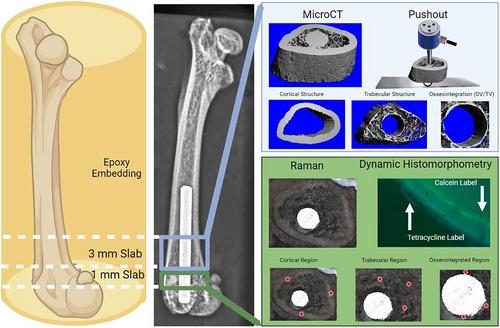
{"title":"Zucker糖尿病- sprague - Dawley大鼠的种植体周围骨形成、基质成分和种植体固定强度受损","authors":"Kyle D Anderson, Christian Beckmann, Saskia Heermant, Frank C Ko, Bryan Dulion, Imad Tarhoni, Jeffrey A Borgia, Amarjit S Virdi, Markus A Wimmer, D Rick Sumner, Ryan D Ross","doi":"10.1002/jbm4.10819","DOIUrl":null,"url":null,"abstract":"<p>An increasing number of patients with type 2 diabetes (T2DM) will require total joint replacement (TJR) in the next decade. T2DM patients are at increased risk for TJR failure, but the mechanisms are not well understood. The current study used the Zucker Diabetic-Sprague Dawley (ZDSD) rat model of T2DM with Sprague Dawley (SPD) controls to investigate the effects of intramedullary implant placement on osseointegration, peri-implant bone structure and matrix composition, and fixation strength at 2 and 10 weeks post-implant placement. Postoperative inflammation was assessed with circulating MCP-1 and IL-10 2 days post-implant placement. In addition to comparing the two groups, stepwise linear regression modeling was performed to determine the relative contribution of glucose, cytokines, bone formation, bone structure, and bone matrix composition on osseointegration and implant fixation strength. ZDSD rats had decreased peri-implant bone formation and reduced trabecular bone volume per total volume compared with SPD controls. The osseointegrated bone matrix of ZDSD rats had decreased mineral-to-matrix and increased crystallinity compared with SPD controls. Osseointegrated bone volume per total volume was not different between the groups, whereas implant fixation was significantly decreased in ZDSD at 2 weeks but not at 10 weeks. A combination of trabecular mineral apposition rate and postoperative MCP-1 levels explained 55.6% of the variance in osseointegration, whereas cortical thickness, osseointegration mineral apposition rate, and matrix compositional parameters explained 69.2% of the variance in implant fixation strength. The results support the growing recognition that both peri-implant structure and matrix composition affect implant fixation and suggest that postoperative inflammation may contribute to poor outcomes after TJR surgeries in T2DM patients. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>","PeriodicalId":14611,"journal":{"name":"JBMR Plus","volume":"7 11","pages":""},"PeriodicalIF":3.4000,"publicationDate":"2023-10-11","publicationTypes":"Journal Article","fieldsOfStudy":null,"isOpenAccess":false,"openAccessPdf":"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10819","citationCount":"0","resultStr":"{\"title\":\"Zucker Diabetic-Sprague Dawley Rats Have Impaired Peri-Implant Bone Formation, Matrix Composition, and Implant Fixation Strength\",\"authors\":\"Kyle D Anderson, Christian Beckmann, Saskia Heermant, Frank C Ko, Bryan Dulion, Imad Tarhoni, Jeffrey A Borgia, Amarjit S Virdi, Markus A Wimmer, D Rick Sumner, Ryan D Ross\",\"doi\":\"10.1002/jbm4.10819\",\"DOIUrl\":null,\"url\":null,\"abstract\":\"<p>An increasing number of patients with type 2 diabetes (T2DM) will require total joint replacement (TJR) in the next decade. T2DM patients are at increased risk for TJR failure, but the mechanisms are not well understood. The current study used the Zucker Diabetic-Sprague Dawley (ZDSD) rat model of T2DM with Sprague Dawley (SPD) controls to investigate the effects of intramedullary implant placement on osseointegration, peri-implant bone structure and matrix composition, and fixation strength at 2 and 10 weeks post-implant placement. Postoperative inflammation was assessed with circulating MCP-1 and IL-10 2 days post-implant placement. In addition to comparing the two groups, stepwise linear regression modeling was performed to determine the relative contribution of glucose, cytokines, bone formation, bone structure, and bone matrix composition on osseointegration and implant fixation strength. ZDSD rats had decreased peri-implant bone formation and reduced trabecular bone volume per total volume compared with SPD controls. The osseointegrated bone matrix of ZDSD rats had decreased mineral-to-matrix and increased crystallinity compared with SPD controls. Osseointegrated bone volume per total volume was not different between the groups, whereas implant fixation was significantly decreased in ZDSD at 2 weeks but not at 10 weeks. A combination of trabecular mineral apposition rate and postoperative MCP-1 levels explained 55.6% of the variance in osseointegration, whereas cortical thickness, osseointegration mineral apposition rate, and matrix compositional parameters explained 69.2% of the variance in implant fixation strength. The results support the growing recognition that both peri-implant structure and matrix composition affect implant fixation and suggest that postoperative inflammation may contribute to poor outcomes after TJR surgeries in T2DM patients. © 2023 The Authors. <i>JBMR Plus</i> published by Wiley Periodicals LLC on behalf of American Society for Bone and Mineral Research.</p>\",\"PeriodicalId\":14611,\"journal\":{\"name\":\"JBMR Plus\",\"volume\":\"7 11\",\"pages\":\"\"},\"PeriodicalIF\":3.4000,\"publicationDate\":\"2023-10-11\",\"publicationTypes\":\"Journal Article\",\"fieldsOfStudy\":null,\"isOpenAccess\":false,\"openAccessPdf\":\"https://asbmr.onlinelibrary.wiley.com/doi/epdf/10.1002/jbm4.10819\",\"citationCount\":\"0\",\"resultStr\":null,\"platform\":\"Semanticscholar\",\"paperid\":null,\"PeriodicalName\":\"JBMR Plus\",\"FirstCategoryId\":\"1085\",\"ListUrlMain\":\"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10819\",\"RegionNum\":0,\"RegionCategory\":null,\"ArticlePicture\":[],\"TitleCN\":null,\"AbstractTextCN\":null,\"PMCID\":null,\"EPubDate\":\"\",\"PubModel\":\"\",\"JCR\":\"Q2\",\"JCRName\":\"ENDOCRINOLOGY & METABOLISM\",\"Score\":null,\"Total\":0}","platform":"Semanticscholar","paperid":null,"PeriodicalName":"JBMR Plus","FirstCategoryId":"1085","ListUrlMain":"https://onlinelibrary.wiley.com/doi/10.1002/jbm4.10819","RegionNum":0,"RegionCategory":null,"ArticlePicture":[],"TitleCN":null,"AbstractTextCN":null,"PMCID":null,"EPubDate":"","PubModel":"","JCR":"Q2","JCRName":"ENDOCRINOLOGY & METABOLISM","Score":null,"Total":0}
引用次数: 0
引用
批量引用

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


