TMPRSS2: COVID-19预后的潜在生物标志物
IF 2.3
4区 医学
Q3 PHARMACOLOGY & PHARMACY
引用次数: 61
摘要
本文章由计算机程序翻译,如有差异,请以英文原文为准。
TMPRSS2: Potential Biomarker for COVID-19 Outcomes.
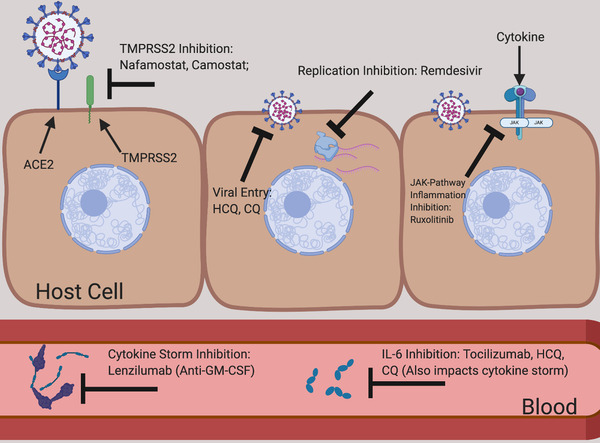
Coronavirus disease 2019 (COVID-19) clinical data has so far shown that the mortality rate for men is higher than for women. This disparity is observed worldwide and across different ethnic/racial groups (Table 1). Early reports from Italy and Germany show that while infection rates are similar between sexes, nearly 70% and 65%, respectively, of deaths aremales. InNewYork City, an epicenter of the US outbreak, 54% of those infected are men, yet men account for 63% of deaths. Epidemiologic data from the previous coronavirus infections, severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS), also indicated sex-based differences in disease susceptibility and outcomes. This discrepancy was attributed tomany factors, including smoking, immune differences, and other comorbidities. An initial report released by the Centers for Disease Control and Prevention (CDC) on population-based surveillance sampled across 14 states, representing 10% of the US population, has indicated that age and comorbidities are associated with increased hospitalization rates of patients with COVID19.1 The data on sex also suggest sexual dimorphism consistent with reports from other countries (Table 1). The preliminary data on race suggest that minority populations may be disproportionately impacted by the coronavirus, where blacks contributed to 33% of the hospitalizations despite representing only 18% of the sampled population. As more data become available, correlations between race and disease severity can be interrogated more thoroughly, including the role of socioeconomic factors on influencing this disparity. Investigations into the genetic and molecular differences between women and men are warranted to identify relevant biomarkers for disease susceptibility and outcomes. Based on data from literature, we propose a novel mechanism of the observed sex differences in clinical outcomes in patients and identify a role for the transmembrane protease serine 2 (TMPRSS2) as a contributing factor to the more severe outcomes noted for COVID-19.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊
CiteScore
5.10
自引率
3.40%
发文量
176
审稿时长
2 months
期刊介绍:
The Journal of Clinical Pharmacology (JCP) is a Human Pharmacology journal designed to provide physicians, pharmacists, research scientists, regulatory scientists, drug developers and academic colleagues a forum to present research in all aspects of Clinical Pharmacology. This includes original research in pharmacokinetics, pharmacogenetics/pharmacogenomics, pharmacometrics, physiologic based pharmacokinetic modeling, drug interactions, therapeutic drug monitoring, regulatory sciences (including unique methods of data analysis), special population studies, drug development, pharmacovigilance, womens’ health, pediatric pharmacology, and pharmacodynamics. Additionally, JCP publishes review articles, commentaries and educational manuscripts. The Journal also serves as an instrument to disseminate Public Policy statements from the American College of Clinical Pharmacology.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


