带状结扎辅助钳-剪刀切断术治疗独特带梗结直肠病变伴茎静脉曲张。
IF 1
Q4 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 0
摘要
本文章由计算机程序翻译,如有差异,请以英文原文为准。
Band Ligation-Assisted Forceps Scissor Transection of a Unique Pedunculated Colorectal Lesion with Stalk Varices.
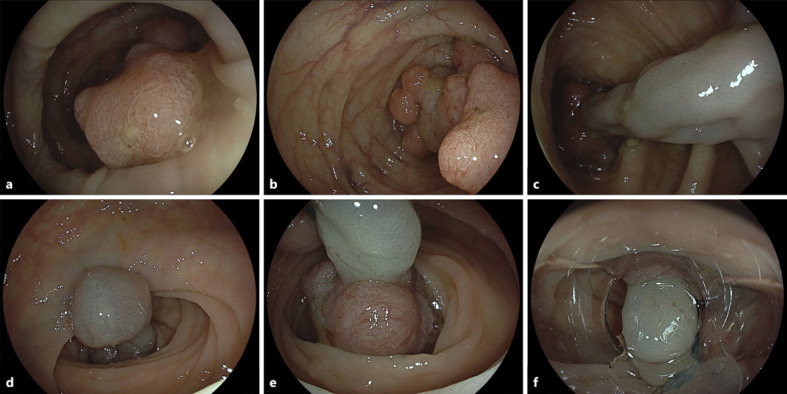
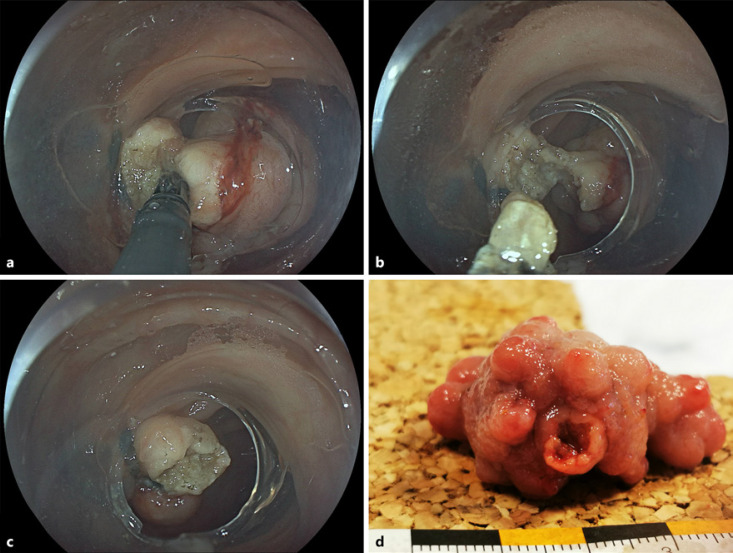
An 81-year-old male patient presented for ileocolonoscopy for anemia workup. While smaller polypoid lesions in the remaining colon were resected without complications, an estimated 50-mm, complex pedunculated (Paris Ip) lesion with a unique multinodular, uneven surface was observed in the sigmoid (Fig. 1a). However, dedicated optical assessment of large areas of the lesion indicated adenoma-typical vessel and surface pattern, albeit full optical assessment of the large and floppy lesion was not feasible (EC760R-V/I; Fuji, Düsseldorf, Germany) (Fig. 1b). More intriguingly, the 25-mm-long and 10-mm-wide stalk demonstrated marked varices originating from adjacent flat sigmoid mucosa (Fig. 1c). Given concerns as to whether adequate placement of a snare and/or prophylactic loop would be feasible in consideration of the large head and markedly uneven surface, in this unique setting we opted for an individual approach, implementing stalk transection after endoscopic band ligation. To this end, we provided the insertion point at 35 cm with two rubber bands as per standard procedure (Fig. 1d, e). Alternatively, clip application at the stalk base might have been discussed for prophylactic hemostasis. However, this was decided against due to, among others, concerns for thermal injury. Cap-fitted gastroscope reinsertion exposed the edematous stalk with the ligations at 6 o’clock and the polyp head at 12 o’clock (Fig. 1f). Next, we completed an uncomplicated forceps scissor transection of the highly fibrotic stalk, using a scissor-type knife device, only at the first cut resulting in self-limited bleeding from ligated varices (Fig. 2a, b). Electrosurgical settings were as follows: transection (mucosa and submucosa): Endocut Q, effect 2, duration 3,
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

GE Portuguese Journal of Gastroenterology
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
1.60
自引率
11.10%
发文量
62
审稿时长
21 weeks
期刊介绍:
The ''GE Portuguese Journal of Gastroenterology'' (formerly Jornal Português de Gastrenterologia), founded in 1994, is the official publication of Sociedade Portuguesa de Gastrenterologia (Portuguese Society of Gastroenterology), Sociedade Portuguesa de Endoscopia Digestiva (Portuguese Society of Digestive Endoscopy) and Associação Portuguesa para o Estudo do Fígado (Portuguese Association for the Study of the Liver). The journal publishes clinical and basic research articles on Gastroenterology, Digestive Endoscopy, Hepatology and related topics. Review articles, clinical case studies, images, letters to the editor and other articles such as recommendations or papers on gastroenterology clinical practice are also considered. Only articles written in English are accepted.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


