INGENIOUS试验:在一项实用的临床试验中,药物遗传学测试对不良事件的影响。
IF 2.9
3区 医学
Q2 GENETICS & HEREDITY
引用次数: 0
摘要
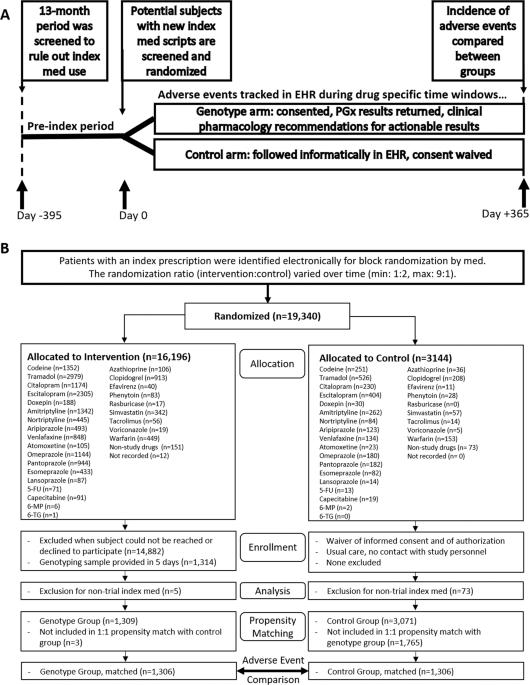
药物不良事件(ADE)造成了显著的死亡率、发病率和成本负担。药物遗传学测试有可能减少ADE和无效性。这项INGENIOUS试验(NCT02297126)分析的目的是确定进行和报告药物遗传学小组测试是否会影响ADE频率。该试验是一项实用的随机对照临床试验,适用于个体的倾向匹配分析(N = 2612)在社区安全网和学术健康系统中接收26种可药用药物中的一种或多种的新处方。干预措施是对26种药物进行药物遗传学测试,并将剂量和选择建议返回健康记录。根据修订的不良事件通用术语标准(CTCAE),主要结果是1年内发生ADE。在倾向匹配分析中,16.1%的个体在1年内经历过任何ADE。严重ADE(CTCAE水平≥ 3) 发生在3.2%的个体中。当联合所有26种药物时,在任何ADE(比值比0.96,95%CI:0.78-1.18)、严重ADE(OR:0.91,95%CI:0.58-1.40)或死亡率(OR:0.60,95%CI:0.28-1.21)方面,药物遗传学测试组和对照组之间没有观察到显著差异。然而,亚组分析显示,在接受阿立哌唑和5-羟色胺或5-羟色胺-去甲肾上腺素再摄取抑制剂药物基因分型的个体中,严重的ADE和死亡减少(or 0.34,95%CI:0.12-0.85)。总之,在药物基因测试后,未观察到总体ADE的变化。然而,INGENIOUS期间发生的限制可能会影响结果。未来的研究可能会考虑先发制人,而不是反应性的药物遗传学小组测试。本文章由计算机程序翻译,如有差异,请以英文原文为准。

The INGENIOUS trial: Impact of pharmacogenetic testing on adverse events in a pragmatic clinical trial
Adverse drug events (ADEs) account for a significant mortality, morbidity, and cost burden. Pharmacogenetic testing has the potential to reduce ADEs and inefficacy. The objective of this INGENIOUS trial (NCT02297126) analysis was to determine whether conducting and reporting pharmacogenetic panel testing impacts ADE frequency. The trial was a pragmatic, randomized controlled clinical trial, adapted as a propensity matched analysis in individuals (N = 2612) receiving a new prescription for one or more of 26 pharmacogenetic-actionable drugs across a community safety-net and academic health system. The intervention was a pharmacogenetic testing panel for 26 drugs with dosage and selection recommendations returned to the health record. The primary outcome was occurrence of ADEs within 1 year, according to modified Common Terminology Criteria for Adverse Events (CTCAE). In the propensity-matched analysis, 16.1% of individuals experienced any ADE within 1-year. Serious ADEs (CTCAE level ≥ 3) occurred in 3.2% of individuals. When combining all 26 drugs, no significant difference was observed between the pharmacogenetic testing and control arms for any ADE (Odds ratio 0.96, 95% CI: 0.78–1.18), serious ADEs (OR: 0.91, 95% CI: 0.58–1.40), or mortality (OR: 0.60, 95% CI: 0.28–1.21). However, sub-group analyses revealed a reduction in serious ADEs and death in individuals who underwent pharmacogenotyping for aripiprazole and serotonin or serotonin-norepinephrine reuptake inhibitors (OR 0.34, 95% CI: 0.12–0.85). In conclusion, no change in overall ADEs was observed after pharmacogenetic testing. However, limitations incurred during INGENIOUS likely affected the results. Future studies may consider preemptive, rather than reactive, pharmacogenetic panel testing.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Pharmacogenomics Journal
医学-药学
CiteScore
7.20
自引率
0.00%
发文量
35
审稿时长
6-12 weeks
期刊介绍:
The Pharmacogenomics Journal is a print and electronic journal, which is dedicated to the rapid publication of original research on pharmacogenomics and its clinical applications.
Key areas of coverage include:
Personalized medicine
Effects of genetic variability on drug toxicity and efficacy
Identification and functional characterization of polymorphisms relevant to drug action
Pharmacodynamic and pharmacokinetic variations and drug efficacy
Integration of new developments in the genome project and proteomics into clinical medicine, pharmacology, and therapeutics
Clinical applications of genomic science
Identification of novel genomic targets for drug development
Potential benefits of pharmacogenomics.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


