186例自发性冠状动脉夹层的初步治疗策略和长期疗效。
IF 2.6
3区 医学
Q2 CARDIAC & CARDIOVASCULAR SYSTEMS
Seminars in Thoracic and Cardiovascular Surgery
Pub Date : 2024-12-01
DOI:10.1053/j.semtcvs.2023.05.001
引用次数: 0
摘要
自发性冠状动脉夹层(SCAD)是急性冠状动脉综合征的一种罕见但重要的非动脉粥样硬化原因。血管重建适应症和SCAD的长期结果仍然是积极研究的领域。我们报告了我们在SCAD的初始管理策略和长期成果方面的经验。我们回顾了1996-2021年在我们机构接受治疗的所有SCAD诊断患者。人口统计学、合并症、临床表现、血管造影结果和管理策略通过图表审查获得。主要结果是心脏死亡、复发/进行性SCAD、随后诊断为充血性心力衰竭或初始治疗后随后/重复血运重建的复合结果。进行未经调整的Kaplan-Meier生存率分析。在我们机构接受治疗的186名SCAD诊断患者中,149名(80%)为女性。134名(72.0%)患者采用药物治疗,43名(23.1%)患者采用经皮冠状动脉介入治疗,9名(4.8%)患者采用冠状动脉搭桥术 年,P = 0.01)、ST段抬高型心肌梗死(67.0%vs34.0%,P本文章由计算机程序翻译,如有差异,请以英文原文为准。
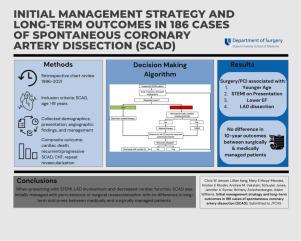
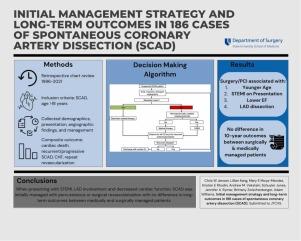
Initial Management Strategy and Long-Term Outcomes in 186 Cases of Spontaneous Coronary Artery Dissection
Spontaneous coronary artery dissection (SCAD) is a rare but important nonatherosclerotic cause of acute coronary syndrome. Indications for revascularization and long-term outcomes of SCAD remain areas of active investigation. We report our experience with initial management strategy and long-term outcomes in SCAD. We reviewed all patients treated at our institution from 1996-2021 with a SCAD diagnosis. Demographics, comorbidities, clinical presentations, angiography findings, and management strategies were obtained by chart review. The primary outcome was a composite of cardiac death, recurrent/progressive SCAD, subsequent diagnosis of congestive heart failure, or subsequent/repeat revascularization after the initial management. Unadjusted Kaplan-Meier survival analysis was performed. Of 186 patients with a SCAD diagnosis treated at our institution, 149 (80%) were female. Medical management was the initial treatment in 134 (72.0%) patients, percutaneous coronary intervention (PCI) in 43 (23.1%), and coronary artery bypass grafting in 9 (4.8%). Surgery/PCI intervention was associated with younger age (38.8 vs 47.7 years, P = 0.01), ST elevation myocardial infarction on presentation (67.0% vs 34.0%, P < 0.001), lower ejection fraction (45.0% vs 55.0%, P = 0.002), and left anterior descending coronary artery dissection (75.0% vs 51.0%, P = 0.006). Ten-year freedom from our composite outcome was similar between revascularized patients and those managed with medical therapy (P = 0.36). Median follow-up time was 4.5 years. SCAD in the setting of ST elevation myocardial infarction, left anterior descending coronary artery involvement, or decreased cardiac function suggests greater ischemic insult and was associated with initial percutaneous or surgical revascularization. Despite worse disease on initial presentation, long-term outcomes of patients undergoing revascularization are similar to medically managed patients with SCAD.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Seminars in Thoracic and Cardiovascular Surgery
Medicine-Pulmonary and Respiratory Medicine
CiteScore
5.80
自引率
0.00%
发文量
324
审稿时长
12 days
期刊介绍:
Seminars in Thoracic and Cardiovascular Surgery is devoted to providing a forum for cardiothoracic surgeons to disseminate and discuss important new information and to gain insight into unresolved areas of question in the specialty. Each issue presents readers with a selection of original peer-reviewed articles accompanied by editorial commentary from specialists in the field. In addition, readers are offered valuable invited articles: State of Views editorials and Current Readings highlighting the latest contributions on central or controversial issues. Another prized feature is expert roundtable discussions in which experts debate critical questions for cardiothoracic treatment and care. Seminars is an invitation-only publication that receives original submissions transferred ONLY from its sister publication, The Journal of Thoracic and Cardiovascular Surgery. As we continue to expand the reach of the Journal, we will explore the possibility of accepting unsolicited manuscripts in the future.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


