在胆总管置入食管支架治疗不能手术的胆道IPMN 1例。
IF 2.4
Q2 GASTROENTEROLOGY & HEPATOLOGY
Therapeutic Advances in Gastrointestinal Endoscopy
Pub Date : 2023-01-01
DOI:10.1177/26317745231183311
引用次数: 0
摘要
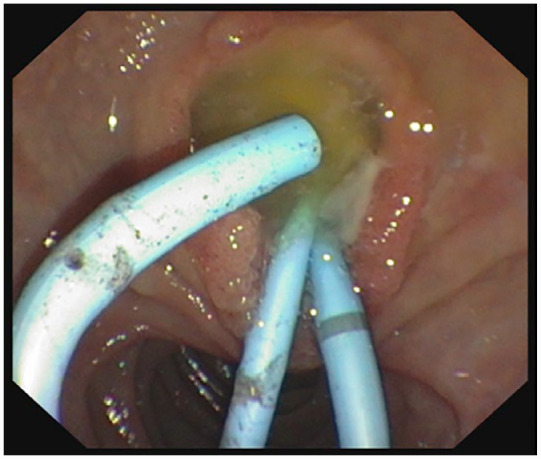
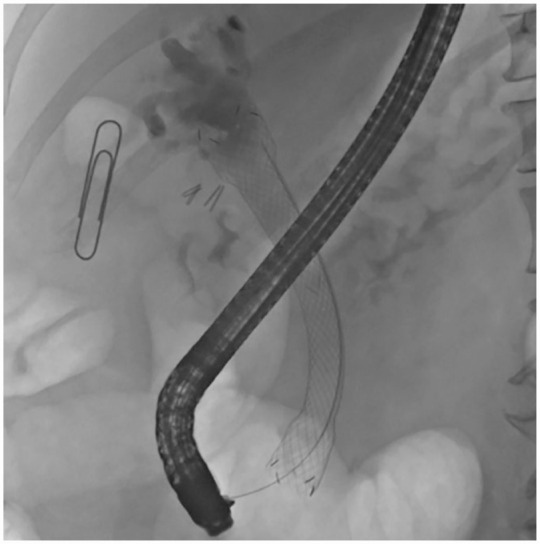
胆道导管内乳头状黏液性肿瘤是一种罕见的胆道肿瘤,最好采用肿瘤切除治疗。内镜射频(RF)消融可作为一种姑息性措施。我们提出一个罕见的病例,其中严重的合并症阻止手术。持续的黏液产生引起严重的胆管炎反复发作。由于复发性胆道梗阻,多次内镜逆行胰胆管造影是必要的。射频消融对无狭窄的扩张胆总管无效。标准胆道支架因移位或闭塞而失败。当其他选择都失败时,我们做出了一个特殊的决定:在ERCP中插入一个覆盖的大直径食管支架到胆管中,以确保胆汁流动并停止粘液的产生。在内镜治疗中,数字胆管镜是标准ERCP的重要辅助手段。姑息治疗方法是成功的:没有支架相关的不良事件或胆管炎再入院。姑息治疗的随访一直持续到患者生命的最后10个月。本文章由计算机程序翻译,如有差异,请以英文原文为准。
Unconventional treatment of inoperable biliary IPMN with an oesophageal stent in the common bile duct: case report.
Biliary intraductal papillary mucinous neoplasm (IPMN) is a rare biliary neoplasia preferably treated with oncologic resection. Endoscopic radio frequency (RF) ablation may be used as a palliative measure. We present a rare case, where heavy co-morbidities prevented surgery. Continuous mucus production caused recurrent episodes of severe cholangitis. Several ERCPs (endoscopic retrograde cholangio pancretography) were necessary due to recurrent biliary obstruction. RF ablation was not effective in the dilated common bile duct without a stricture. Standard biliary stents failed due to either migration or occlusion. When other options failed, an exceptional decision was made: a covered large diameter oesophageal stent was inserted in ERCP into the bile duct to secure bile flow and stop mucus production. Digital cholangioscopy was crucial adjunct to standard ERCP in endoscopic management. The palliative treatment method was successful: there were no stent-related adverse events or readmissions for cholangitis. The follow-up in the palliative care lasted until patient’s last 10 months of lifetime.
求助全文
通过发布文献求助,成功后即可免费获取论文全文。
去求助
来源期刊

Therapeutic Advances in Gastrointestinal Endoscopy
GASTROENTEROLOGY & HEPATOLOGY-
CiteScore
4.80
自引率
0.00%
发文量
8
审稿时长
13 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


