Endovascular Aneurysm Repair Using the ALTO Endograft in a Patient with a Very Tight 10-mm Aortic Bifurcation.
IF 0.8
Q4 PERIPHERAL VASCULAR DISEASE
引用次数: 0
Abstract
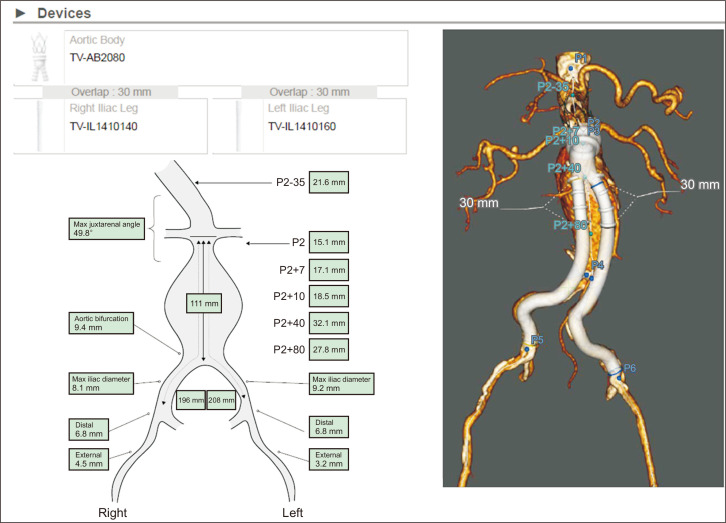
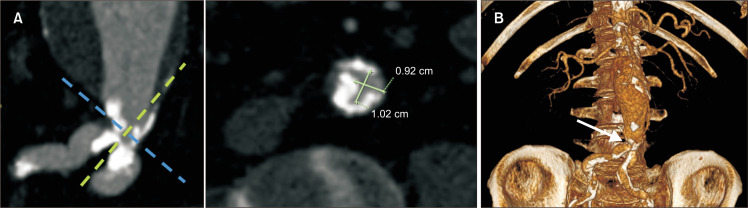
Endovascular aneurysm repair (EVAR) is the primary treatment modality for abdominal aortic aneurysms; however, a suitable anatomy is a prerequisite for optimal outcomes. Proximal neck anatomic configuration, including length followed by size and angulation, is the main morphometric characteristic that determines EVAR suitability. Iliac landing zone and access vessels’ adequacy should also be considered [1]. Another characteristic that may affect EVAR feasibility but has received less attention is the presence of a narrow aortic bifurcation (NAB). Data on EVAR outcomes in patients with NAB are scarce and heterogeneous. Overall, EVAR in patients with NAB has been reported to present outcomes similar to those in patients with a standard aortic bifurcation at the expense of considerably more iliac limb stentings and overall adjunctive manipulations during the primary procedure [2,3]. Regarding the definition of NAB, most relevant studies have used a threshold of <20 mm, although <18 mm and <16 mm thresholds have also been used [3]. We report a patient with a very tight 10-mm aortic bifurcation who was successfully treated with an ALTO (Endologix Inc.) endograft (Fig. 1, 2). In this case, simultaneous deployment of the iliac limbs was performed, in contrast to the standard technique in which the contralateral limb is deployed first. Specifically, the

应用ALTO血管内移植物修复10毫米主动脉分叉狭窄患者的血管内动脉瘤。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊

Vascular Specialist International
Medicine-Surgery
CiteScore
1.10
自引率
11.10%
发文量
29
审稿时长
17 weeks
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


