Experiences of a cognitive behavioural therapy (CBT) intervention for fatigue in patients receiving haemodialysis
Abstract
Background
A feasibility randomised-controlled trial found that a cognitive-behavioural therapy intervention for renal fatigue has the potential to reduce fatigue in patients receiving haemodialysis, but uptake was low.
Objectives
Nested in the randomised-controlled trial (RC) qualitative interviews were undertaken to understand the acceptability of renal fatigue, the facilitators of, and barriers to, engagement, and the psychosocial processes of change.
Design
The trial included 24 participants at baseline. Semi-structured interviews were conducted with nine participants from the intervention arm (n = 12). Approach Interviews were carried out immediately following treatment (3 months post-randomisation). Data were analysed using inductive thematic analysis.
Findings
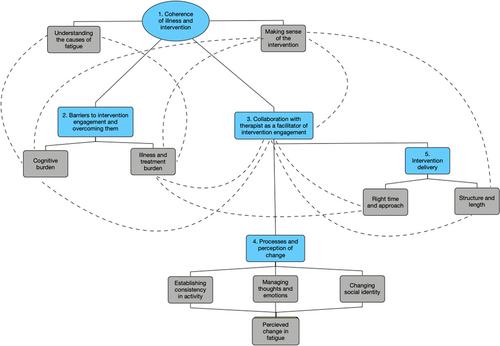
Five main themes were formulated. The overarching theme was a sense of coherence (whether the illness, symptoms and treatment made sense to individuals), which appeared to be central to acceptability and engagement. Two themes captured the key barriers and facilitators to engagement, cognitive and illness/treatment burdens and collaboration with the therapist. Participants described changes related to their activity, thoughts and social identity/interactions, which shaped perceptions of change in fatigue. Lastly, participants discussed the optimal delivery of the intervention.
Conclusions
This study revealed the importance of patients' understanding of fatigue and acceptance of the treatment model for the acceptability of and engagement with a cognitive-behavioural therapy-based intervention for fatigue. Overall, there was an indication that such an intervention is acceptable to patients and the mechanisms of change align with the proposed biopsychosocial model of fatigue. However, it needs to be delivered in a way that is appealing and practical to patients, acknowledging the illness and treatment burdens.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


