Atezolizumab and Bevacizumab Combination Therapy and Sequential Conversion Hepatectomy for Advanced Fibrolamellar Hepatocellular Carcinoma Presenting Pseudoprogression.
IF 11.6
1区 医学
Q1 GASTROENTEROLOGY & HEPATOLOGY
引用次数: 1
Abstract
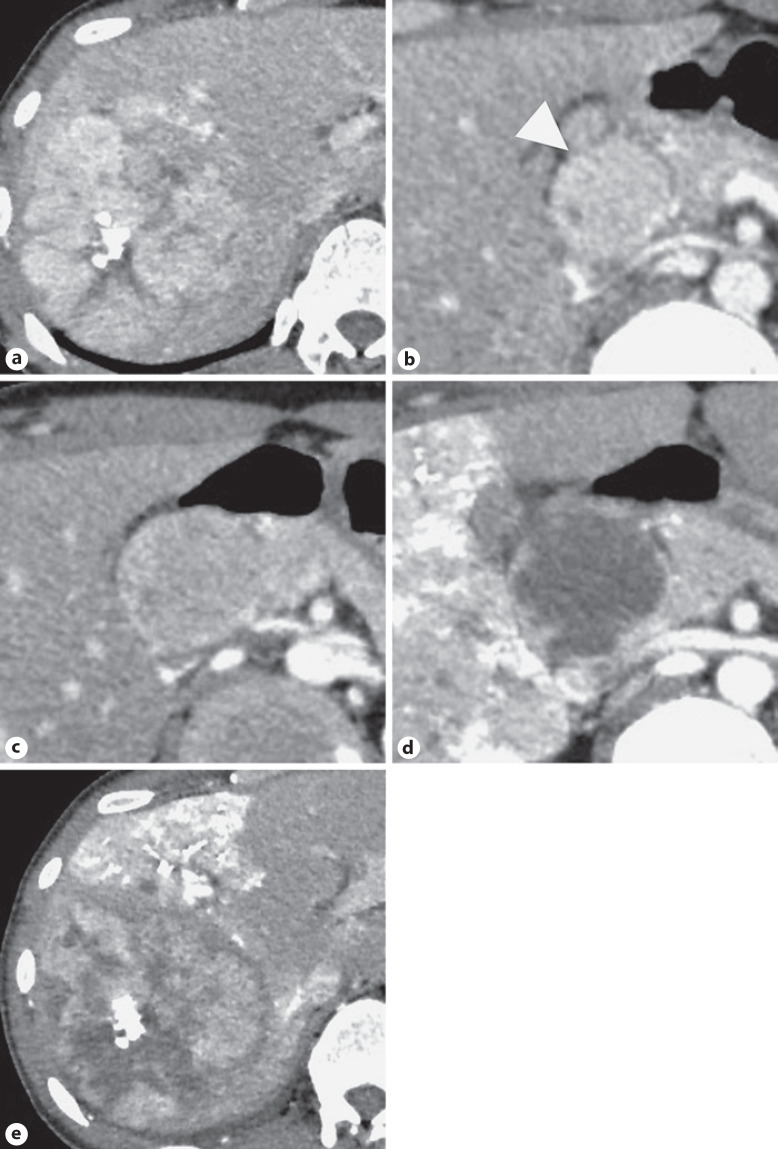
Fibrolamellar hepatocellular carcinoma (FLHCC) is a rare a rare subtype of hepatocellular carcinoma. The IMbrave150 trial demonstrated that atezolizumab and bevacizumab therapy (ABT) has better treatment outcomes than sorafenib for advanced HCC. However, since patients with known FLHCC were excluded from this trial, the effects of ABT on FLHCC remain unknown. We report the first case of ABT for advanced FLHCC followed by hepatectomy presenting pseudoprogression of lymph node (LN) metastases which was pathologically proven after surgery. The patient was a 30-year-old man with advanced FLHCC and multiple LN metastases behind the pancreatic head, and ABT was introduced. After four courses of treatment, CT indicated a minor decrease in the intratumor vascularity of the liver tumor. However, the size of metastatic LNs increased. Subsequently, the patient presented with bloody stool, and colonoscopy revealed immune-related colitis caused by atezolizumab. Therefore, the fifth course was canceled. A right hemihepatectomy following percutaneous transhepatic portal vein embolization (PTPE) was performed to increase the future liver remnant volume. After PTPE, dynamic CT revealed an objective response to ABT; SD in RECIST 1.1 (7% increase in the LN size and no change of liver tumor), and PR in modified RECIST (47% decrease in the intratumor vascularity of the liver tumor and LNs). Three weeks after PTPE, right hemihepatectomy plus nodal dissection was successfully performed. Pathological findings revealed that approximately 60%–70% of the liver tumor and 70%–80% of the metastatic LNs were necrotic, indicating a good response to ABT. The increasing size of metastatic LNs that occurred during the treatment course was deemed pseudoprogression. Pseudoprogression can be found in patients with solid malignancies treated with immune checkpoint inhibitors, however, rarely occurs in HCC. The first response to metastatic LNs was observed 20 weeks after ABT initiation combined with an increase in nodal volume and a decrease in vascularity. In the updated data of the IMbrave150 trial, 19% of the first responses occurred after week 24. Physicians should consider that ABT may also be effective in FLHCC and may cause pseudoprogression before determining a treatment strategy.

阿特唑单抗和贝伐单抗联合治疗和顺序转换肝切除术治疗出现假进展的晚期纤维板层性肝细胞癌。
本文章由计算机程序翻译,如有差异,请以英文原文为准。
求助全文
约1分钟内获得全文
求助全文
来源期刊
Liver Cancer
Medicine-Oncology
CiteScore
20.80
自引率
7.20%
发文量
53
审稿时长
16 weeks
期刊介绍:
Liver Cancer is a journal that serves the international community of researchers and clinicians by providing a platform for research results related to the causes, mechanisms, and therapy of liver cancer. It focuses on molecular carcinogenesis, prevention, surveillance, diagnosis, and treatment, including molecular targeted therapy. The journal publishes clinical and translational research in the field of liver cancer in both humans and experimental models. It publishes original and review articles and has an Impact Factor of 13.8. The journal is indexed and abstracted in various platforms including PubMed, PubMed Central, Web of Science, Science Citation Index, Science Citation Index Expanded, Google Scholar, DOAJ, Chemical Abstracts Service, Scopus, Embase, Pathway Studio, and WorldCat.
 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


