Building local decision-making competencies during COVID-19: Accelerating the transition from learning healthcare systems to learning health communities
Abstract
Introduction
The persisting and evolving COVID-19 pandemic has made apparent that no singular policy of mitigation at a regional, national or global level has achieved satisfactory and universally acceptable results. In the United States, carefully planned and executed pandemic policies have been neither effective nor popular and COVID-19 risk management decisions have been relegated to individual citizens and communities. In this paper, we argue that a more effective approach is to equip and strengthen community coalitions to become local learning health communities (LLHCs) that use data over time to make adaptive decisions that can optimize the equity and well-being in their communities.
Methods
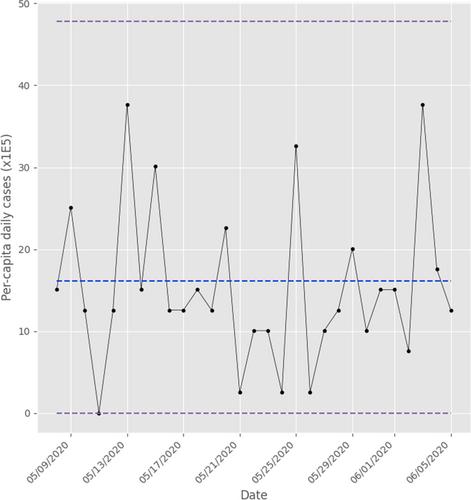
We used data from the North Carolina (NC) county and zip code levels from May to August 2020 to demonstrate how a LLHC could use statistical process control (SPC) charts and simple statistical analysis to make local decisions about how to respond to COVID-19.
Results
We found many patterns of COVID-19 progression at the local (county and zip code) levels during the same time period within the state that were completely different from the aggregate NC state level data used for policy making.
Conclusions
Systematic approaches to learning from local data to support effective decisions have promise well beyond the current pandemic. These tools can help address other complex public health issues, and advance outcomes and equity. Building this capacity requires investment in data infrastructure and the strengthening of data competencies in community coalitions to better interpret data with limited need for advanced statistical expertise. Additional incentives that build trust, support data transparency, encourage truth-telling and promote meaningful teamwork are also critical. These must be carefully designed, contextually appropriate and multifaceted to motivate citizens to create and sustain an effective learning system that works for their communities.

 求助内容:
求助内容: 应助结果提醒方式:
应助结果提醒方式:


